Acquired thrombotic thrombocytopenic purpura (TTP) is a rare, fatal thromboticmicroangiopathy with an estimated incidence of three cases per 1,000,000 adults per year. It is caused by severely reduced activity of von-Willebrand factor (vWF)-cleaving protease ADAMTS13 (a disintegrin-like and metalloprotease with thrombospondin type 1motif no. 13’). The disease manifests as thrombocytopenia, hemolyticanemia, and organ failure. Its etiology is unclear, although it has been linked to various conditions such as sepsis, autoimmune disorders, malignancies, and pregnancy. We report a rather rare presentation of acquired TTP triggered by acute pancreatitis.
Case Report
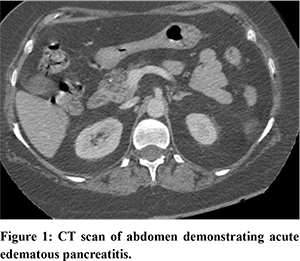
A 60-year-old female patient presented to the emergency department with complaints of severe epigastric pain and vomiting for last 3 days. Pain was moderate to severe in intensity, radiating to back. There was no history suggestive of sub-acute intestinal obstruction, alcohol intake, biliary colic or fever. The patient was a known diabetic and hypertensive on metformin and calcium channel blockers. Physical examination was notable only for epigastric tenderness. Initial laboratory parameters were suggestive of acute pancreatitis (elevated amylase- 1800 units/L and lipase- 1328 units/L), normal liver function test, lipid profile, serum calcium and phosphate level (Bilirubun-0.7, aspartate transaminase-33, alanine transaminase-38, alkaline phosphatase-121, triglyceride-138, low density lipoprotein-104, calcium=8.3, phosphate- 2.3). There was also anaemia with thrombocytopenia (Hb-9.8 gm/dl, TLC-6400, PLT-94000/microL), initially which was contributed to a manifestation of undiagnosed viral infection.Ultrasonography of abdomen suggested that pancreas was bulky, there was no evidence of gall stone or cholecystitis, and normal common bile duct. Acute pancreatitis was managed with intravenous hydration and opioid analgesics. Although the patient improved symptomatically over the next 2 days, she developed acute kidney injury (serum creatinine-2.1 mg/dl) and further worsening of anemia and thrombocytopenia (Hb- 6.8 gm/dl, PLT- 18000 /microL), NCCT abdomen was suggestive of acute edematous pancreatitis with peripancreatic inflammatory changes (Figure 1). On further evaluation, she found to have evidence of hemolysis (LDH- 805 U/L, haptoglobin <30 mg/dl; (range 36-195 mg/dl), schistocytes in peripheral smear). Normal serum procalcitonin, imaging and blood culture report ruled out any evidence of sepsis, or malignancy. PT, INR and aPTT were within normal range. A presumptive diagnosis of TTP was made on the basis of this clinical scenario. PLASMIC score was 6, indicating a high risk (72%) of severe ADAMTS13 deficiency.
Patient was started on IV steroid and plasmapheresis, which resulted in prompt improvement in her blood count and AKI. During hospital stay, she also developed neurological symptoms (unilateral numbness and weakness of limbs). After neurology consultation MRI brain was done which was suggestive of acute ischemic injury. She was treated with 5 sessions of plasmapheresis, in addition to intravenous steroids and supportive blood transfusions. But as plasmapheresis stopped, the patient was again found to have a drop in Hb, so the patient was put on injection rituximab (weekly)in view of persistent need for plasmapheresis and neurological symptoms. Her initial ADAMTS13 level was very low, serial ADAMTS13 level showed gradual improvement. Once ADAMTS13 came to normal level steroids were tapered. Patient was discharged in stable condition and was given a total of 4 doses of weekly rituximab to prevent relapse.
Discussion
VWF is a large glycoprotein produced in endothelial cells,megakaryocytes, and subendothelial connective tissue. It binds to platelet GP1b-IX-V receptor complex and subendothelialcollagen, resulting in platelet adhesion to the endothelium as well as platelet GPIIb/IIIareceptors, allowing platelet-platelet aggregation. Shear stress in arteriolar and capillarycirculation triggers vWF and platelets to form aggregates.The endothelial vWF polymer is cleaved into multimers of progressively smaller size byADAMTS13, a plasma metalloprotease1.
Inflammatory conditions can decrease in ADAMTS13 activity by transcriptional down regulation, proteolytic degradation, and consumption due to the high plasma VWF levels. ReducedADAMTS13 activity results in abnormalities in vWF multimer quantities and patterns, leadingto a prothrombotic state. Endothelial injury and platelet aggregation cause the formation of platelet thrombi in terminal arterioles and capillaries resultingin hemolytic anemia and thrombocytopenia1,2. The classic‘pentad’ of microangiopathic hemolyticanemia (MAHA), thrombocytopenia, fever, acute renal failure, and neurologic abnormalities are rare, found only in less than 5% of patients.
While pancreatic involvement in TTP is an established entity, acute pancreatitis as an inciting event of TTP is sparsely reported, with only 11 case reports and two case series found in our literature review. Swisher et al. in a review of five such cases, found a median interval of three days between the diagnosis of acute pancreatitis and TTP, corresponding to the timeline in this patient. Another review of such cases from a regional TTP registry in UK also found a median interval of three days. In both case series, pancreatitis was resolving when the signs of TTP first appeared.
Acute pancreatitis triggers a systemic inflammatory response with increased plasma levels of cytokines such as tumor necrosis factor-a (TNF-a), interleukin (IL)-1, IL-6, and IL-88,9. These pro-inflammatory cytokines cause endothelial injury, which in turn has been postulated as a causative mechanism of TTP. IL-8 and TNF-a stimulate the release of the ultra-large form of vWF from the endothelium in in-vitro studies. Additionally, IL-6 inhibits cleavage of ultra-large vWF by ADAMTS13 under shear stress3. Several studies demonstrated elevated vWF in acute pancreatitis3. Morioka et al. reported increased concentrations of vWF with low activity of ADAMTS13 among 13 severe acute pancreatitis patients without disseminated intravascular coagulation (DIC). Increased vWF concentrations positively correlated with the severity of organ failure, APACHE III scores, and sequential organ failure assessment (SOFA) scores. Development of TTP could be a consequence of the elevated VWF level and decreased ADAMTS13 activity caused by a systemic inflammatory state associated with pancreatitis.
Due to therarity of this association, it is difficult to delineate the exact chain of events; and further research is needed on this association.Thrombocytopenia and hemolytic anemia, were the early clues. The PLASMIC score is a useful tool to predict the likelihood of TTP. This scoring system is highly sensitive and is superior to standard clinical judgement in predicting severe ADAMTS13 deficiency, assisting in the diagnostic challenge ofTTP4. Severely deficient ADAMTS13 activity supports the diagnosis but has a long turnaround time. Therapy is initiated based on clinical diagnosis. Plasma exchange (PLEX) is the mainstay of therapy5. Glucocorticoids and rituximab improve outcomes and reduce the duration of plasma exchange. Early initiation of plasmapheresis is key to the clinical outcome and survival rates are excellent in such cases.
Conclusions
Acute pancreatitis is a well-documented consequence of TTP. However, acute pancreatitis leading to TTP is rarely reported. Systemic inflammation associated with acute pancreatitis appears to be involved in the pathogenesis of TTP in these cases. Thrombocytopenia and hemolytic anemia are the most consistent early findings in the majority of reported cases. The classic description of TTP ‘pentad’ or ADMATS13 activity assay are not reliable in making a diagnosis sufficiently early in the disease process. Early diagnosis and treatment results in favourable clinical outcome.
References
- Tsai H-M. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol.2010;91:1-19.
- Tsai H-M, Lian EC-Y: Antibodies to von willebrand factor-cleaving protease in acutethrombotic thrombocytopenic purpura. N Engl J Med. 1998;339:1585-94.
- Siemiatkowski A, Wereszczynska-Siemiatkowska U, Mroczko B, Galar M, Maziewski T. Circulating endothelial mediators in human pancreatitis-associated lung injury.Eur JGastroenterol Hepatol. 2015, 27:728-734.
- Bendapudi PK, Hurwitz S, Fry A, et al.: Derivation and external validation of the PLASMICscore for rapid assessment of adults with thrombotic microangiopathies: a cohort study.Lancet Haematol. 2017;4:e157-e164.
- Rock GA, Shumak KH, Buskard NA, et al. Comparison of plasma exchange with plasmainfusion in the treatment of thrombotic thrombocytopenic purpura. N Engl J Med. 1991;325:393-97.