48uep6bbphidcol2|ID
48uep6bbphidvals|1934
48uep6bbph|2000F98CTab_Articles|Fulltext
Abdominal TB has been reported in 11-16% cases with extra pulmonary cases1. Isolated pancreatic involvement is rare in both immunocompetent and immunocompromised conditions2. Here we report a case of pancreatic SOL (space occupying lesion), suspected as solid cystic lesion of pancreas on imaging, which was finally diagnosed as pancreatic tuberculosis.
Case Report
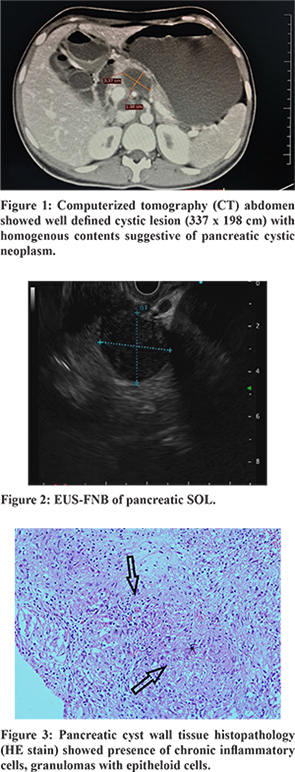
We report a case of 24-year-old female with no known co-morbidities who was evaluated for unintentional weight loss. She lost 12 kg weight in 1-year duration and had complaints of easy fatigability and occasional pain abdomen. She never had fever, altered bowel habits, cough or chest pain. On evaluation her hematological profile showed low haemoglobin (9.6 gram%, MCV 83fl) and normal leucocyte and platelet counts. Liver and renal profiles were within normal limits. Erythrocyte sedimentation rate was on higher side (60 mm in 1st hr). In view of abdomen pain, ultrasound abdomen was performed and found to have heterogenous hypoechoic lesion superior to and abutting body of pancreas along with evidence of cholelithiasis. Markers for malignancy were negative (CEA, CA 19-9). Computerized tomography (CT) abdomen showed well-defined cystic lesion (3.37 × 1.98 cm) with homogenous contents arising from superior margin of pancreas and irregular wall thickening / soft tissue component in posterio superior aspect of lesion with no inflammatory fat stranding or calcification suggestive of pancreatic cystic neoplasm (Figure 1). She underwent endoscopic ultrasoundguided fine needle biopsy (EUS-FNB), but tissue examination was inconclusive despite presence of adequate tissue. Repeated EUS-FNB also did not give diagnosis. Later diagnostic laparoscopy was performed. Intraoperatively supra-pancreatic cyst of 3.5 × 3 cm lesion noted. On opening of the cyst wall, whitish cheese caseous material noted and about 25 ml of material aspirated. Cyst wall showed necrosis. Cystic material was biopsied. Tissue was sent for histopathology examination (HPE), acid fast bacilli (AFB) culture and MTB Gene Xpert. Pancreatic cyst wall tissue HPE revealed presence of chronic inflammatory cells, granulomas with epitheloid cells (Figure 3). MTB Gene Xpert of cyst material was found positive. With these findings she was diagnosed as isolated pancreatic tuberculosis started on 4 drug anti tubercular regimen. She improved clinically well and started gaining weight.
Discussion
Primary pancreatic tuberculosis is an unusual manifestation and its almost always a histological surprise. In the absence of other manifestations of Koch’s it is very difficult to suspect isolated TB infection in pancreatic lesions. It may mimic pancreatic malignancy, other cystic lesions of pancreas or autoimmune pancreatitis. Involvement of pancreas by mycobacterium can be due to lympho-hematogenous spread or from adjacent organs3. There is no literature regarding the typical presentation of pancreatic TB, due to its rarity. Few authors denote that it may present as pain abdomen, weight loss or fever episodes. Radiological features are non-specific, may masquerade as neoplastic lesions, which may sometimes warrant major surgical intervention on suspicion of malignancy4. Pombo et al. studied imaging features of 6 patients with pancreatic TB and found three patterns of lesions i.e. mass forming, diffuse and small nodular type5. Among all mass forming type was most common. Our patient also presented with loss of weight and fatigue and found to have mass forming lesion in body of pancreas. EUS-FNB is a safe and promising method for the diagnosis of pancreatic/peripancreatic TB. In a retrospective analysis done in Korean study by Song et al, it was found that EUS-FNB gave diagnosis in 76.2% patients (16 out of 21)6. However, in our patient EUS-FNB examination was inconclusive. Laparoscopy will help whenever there is diagnostic dilemma. Along with tissue sampling, other tissue involvement can be visualized on laparoscopy. Along with tissue sampling, other tissue involvement can be visualized on laparoscopy. Presence of caseating granulomas on histopathology, demonstration of TB bacilli on ZN stain, culture or GeneXpert positivity are diagnostic features. Abdominal tuberculosis responds well to anti tubercular treatment unless it is a drug resistant scenario. It is recommended to give 6 months course of anti-tubercular treatment (ATT) for abdominal TB7. Our patient symptomatically responded well to ATT and she is on follow up now.
Conclusion
Pancreatic tuberculosis is very rare, but whenever there is diagnostic dilemma in a pancreatic SOL, tuberculosis should be considered before planning surgery with the suspicion for neoplastic lesion.
References
- Khan R, Abid S, Jafri W, et al. Diagnostic dilemma of abdominal tuberculosis in non-HIV patients: an ongoing challenge for physicians. World J Gastroenterol 2006;12:6371-5.
- Elizondo ME, Arratibel JA, Compton CC, Warshaw AL. Tuberculosis of pancreas. Surg 2001;129 :114-6.
- Singh DK1, Haider A, Tatke M, Kumar P, Mishra PK. Primary pancreatic tuberculosis masquerading as a pancreatic tumor leading to Whipple’s pancreaticoduodenectomy. A case report and review of the literature. JOP. 2009;10(4):451-6.
- Pombo F, DíazCandamio MJ, Rodriguez E, Pombo S. Pancreatic tuberculosis: CT findings. Abdom Imaging 1998;23:394-397.
- Pombo F, DíazCandamio MJ, Rodriguez E, Pombo S. Pancreatic tuberculosis: CT findings. Abdom Imaging 1998;23:394-7.
- Song TJ, Lee SS, Park DH, Lee TY, Lee SO, Seo DW et al. Yield of EUS-guided FNA on the diagnosis of pancreatic/peripancreatic tuberculosis. GastrointestEndosc. 2009;69:484-91.
- Index TB guidelines for extra pulmonary tuberculosis in India. Chapter 15. Page 63. https://tbcindia.gov.in/showfile.php?lid=3245. (browsing done on 05-08-2018).