48uep6bbphidcol2|ID
48uep6bbphidvals|1826
48uep6bbph|2000F98CTab_Articles|Fulltext
Case Report
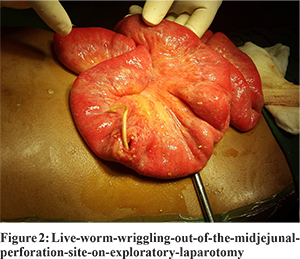
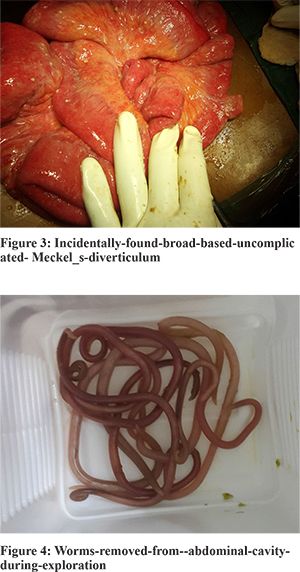
A 17 years old male was brought to the emergency department with a history of trivial assault to the abdomen. He had severe abdominal pain with multiple episodes of non-bilious vomiting. On examination, the patient had tachycardia and hypotension. Diffuse tenderness and guarding was present throughout the abdomen. An erect X-ray of the abdomen showed free gas under the diaphragm. Ultrasonography showed moderate free fluid with moving internal echoes in the abdomen. Diagnostic tap revealed yellow colored bilious aspirate. On emergency exploratory laparotomy, gross bilious contamination was present with multiple live worms floating freely in the abdominal cavity. A small mid-jejunal perforation with pouting mucosa and a live worm wriggling out of it was found. Incidentally, a broad base Meckel’s diverticulum was also discovered. The jejunum distal to the perforation was loaded with worm bolus, which was dislodged and milked out proximally through the perforation. Primary repair of the jejunal perforation was done in two layers, thorough lavage was performed and the abdomen closed over a drain after confirming hemostasis. Patient vomited a live worm in the postoperative period. and To complete deworming, he was started on anti - helminthic therapy. The patient recovered completely and was discharged on the 10th day. At 6 months follow up, patient is asymptomatic with no history of passage of worms in stools and no evidence of ova on stool examination.

Discussion
Ascaris lumbricoides is the most common helminthic infection worldwide with maximum prevalence in tropical countries. Asia alone bears the burden of 73% of the infection with infectivity rate as high as 95% in some population. Ascariasis has varied clinical presentations but generally runs a benign indolent course. Delay in management and incomplete therapy can lead to surgical complications like worm bolus obstruction, appendicitis, pancreatitis and liver abscess. Though rare, perforation peritonitis is a known complication of ascariasis. In most of these cases, co - existing bowel pathologies like typhoid, amoebiasis, meckels diverticulitis, ischemic necrosis due to volvulus and trauma play a synergistic role in causing the perforation.1,2
Ahi K S et al have reported a similar case of intestinal ascariasis with jejunal perforation after trivial trauma.3 Refeidi A has reported a case of the migration of a single live round worm into the peritoneal cavity through a perforation in the duodenum.2 Bowel perforation is thought to follow ischemia from pressure by the mass of worms in the ileum.1 Efem has however postulated that except in confined spaces like the appendix, Meckel’s diverticulum and the biliary tree, the intestine is capable of immense dilatation so as to accommodate up to 5000 worms without symptoms.4
Injury to the intra-abdominal structures is primarily by either compression forces or deceleration forces. The compressive forces may deform hollow organs and transiently increase intraluminal pressure, resulting in rupture. Deceleration forces cause stretching and linear shearing between relatively fixed and free objects.5 In our case it is suggested that trauma might have precipitated animpending perforation due to ascariasis.
Albendazole 400 mg singledose orally is the drug of choice. Alternative drugs like mebendazole, pyrantel pamoate and ivermectin are available. Albendazole is not recommended during pregnancy; pyrantel pamoate is the drug of choice in these cases. Paralyzing vermifuges (eg, pyrantel pamoate, piperazine, ivermectin) should be avoided in patients with complete or partial intestinal obstruction since the paralyzed worms may necessitate or further complicate surgery. In such cases albendazole and mebendazole are preferred. If the patient lives in an endemic area or has recently relocated, he or she may still be carrying larvae that are not yet susceptible. Such patients should be re-evaluated in 3 months and retreated if stool ova persist. In endemic areas, reinfection rates approach 80% within 6 months.
References
- Mishra PK, Agrawal A, Joshi M, Sanghvi B, Shah H et al. Intestinal obstruction in children due to ascariasis:A tertiary health centerexperience. Afr J Paediatr Surg 2008;5:65-70.
- Refeidi A. Live ascaris lumbricoides in the peritoneal cavity. Ann Saudi Med 2007;27:118-21.
- Ahi KS, Munghate A, Chauhan M, Singh H, Kumar A. Ascaris intestinal perforation after trivial trauma.International journal of case reports and images 2014;5(2):165-168.
- Efem EE. Ascaris lumbricoides and intestinal perforation. Br J Surg 1987; 74: 683-4.
- Mukhopadhyay M.Intestinal Injury from Blunt Abdominal Trauma: A Study of 47 Cases.Oman Medical Journal 2009; 24(4):256-259.