48uep6bbphidcol2|ID
48uep6bbphidvals|1755
48uep6bbph|2000F98CTab_Articles|Fulltext
Histoplasmosis is the most common endemic mycosis in the United States.
1 In Brazil its incidence is largely unknown, although it occurs in all regions, with a higher frequency of outbreaks in Rio de Janeiro state.
2 It is caused by Histoplasma capsulatum, which is a thermally dimorphic fungus, growing in a filamentous mycelial form in the soil and as an encapsulated yeast at 37°C or higher in the body. The fungus is found in contaminated soil from bird or bat guano. The highest concentration of the fungus often is in abandoned buildings and caves. Initial exposure is via inhalation, and spread occurs within macrophages through the reticuloendothelial system.
3 Disseminated infection occurs via lymphohematogenous spread of yeast-filled macrophages into nearby lymph nodes and multiple organs, most commonly the liver, spleen, bone marrow, adrenal glands, and gastrointestinal (GI) tract. While GI involvement is not uncommon in patients with disseminated disease, GI histoplasmosis rarely comes to clinical attention due to the lack of specific signs and symptoms.
3 The purpose of this study is to describe the second reported case of upper GI bleeding due to duodenal histoplasmosis in a patient with systemic lupus erythematosus (SLE).
Case Report
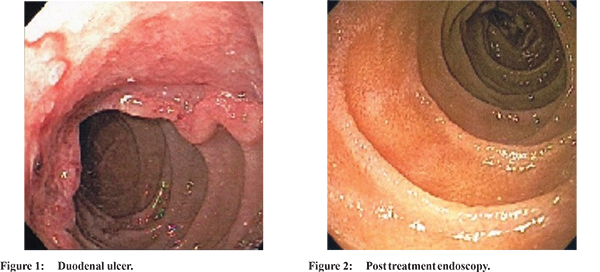
The patient was a 43-year-old female with SLE diagnosed 5 years ago which was undergoing low dose continuous corticosteroid therapy for the last 24 months with prednisone 5 mg per day. She also had a chronic nephropathy secondary to lupus nephritis, with no need for dialysis. She presented to the Emergency sector reporting two episodes of haematemesis and melanotic stools. At physical examination, her mucous was severely pallor; pulse rate was 112 bpm, blood pressure was 110/70 mmHg, and respiratory rate was 24. Thorax and abdomen evaluation revealed no abnormalities. At rectal examination, melanotic stool residues were observed. Laboratory studies revealed severe normochromic normocytic anemia (hemoglobin: 6.1; hematocrit: 20%); coagulation tests, white blood cell and platelet count were normal. An upper GI endoscopy was carried out and revealed an ulcer on the duodenal bulb with signs of recent bleeding (Figure 1). Local therapy with adrenalin injection was performed. Patient received a unity of red blood cells and therapy with intravenous omeprazole was initiated at the dose of 40 mg each 12 hours. Patient presented no more episodes of exteriorized bleeding. After 48 hours, oral nutrition was reintroduced. Hemoglobin stabilized at 8.2 and hematocrit at 29%. Patient was discharged with oral omeprazole 40 mg twice a day for 12 weeks and prednisone was reintroduced. Histological examination of duodenal ulcer showed a chronic granulomatous inflammatory process with presence of Histoplasma capsulatum. No other sites of Histoplasma infection were identified after careful investigation. Oral itraconazole was introduced at the dose of 200 mg twice a day for 12 months. Further investigation for other immunodeficiencies found no abnormalities. Following itraconazole therapy, an upper GI endoscopy revealed no abnormalities (Figure 2). Patient has been followed for 24 months with no further related symptoms or changes.
Discussion
Invasive fungal infections (IFI), including disseminated histoplasmosis, are uncommon in SLE. The reported incidence of IFI in SLE ranges from 0.64% to 1.04%, approximately one case per year.
4 According to the current knowledge, this is the first reported case of GI involvement in such circumstance. Even other manifestations of histoplasmosis in individuals with SLE are also rare and just 17 cases were reported prior to this, and in the majority, pulmonary and skin symptoms predominated.
4,5 In most of the cases that were reviewed, SLE patients who developed histoplasmosis were on long-term immunosuppression, most commonly corticosteroids. These findings suggest that corticosteroids increase the risk of developing histoplasmosis in SLE patients.
4 Corticosteroids seem to affect multiple steps necessary for cellular immunity, including antigen processing, lymphocyte activation and proliferation, response to mediators, and cell-mediated toxicity.
4 Most cases of histoplasmosis are Aids-related.
1-3 In patients with disseminated histoplasmosis, the GI tract is one of the most commonly affected organ systems with approximately 70% of patients demonstrating some GI involvement at autopsy. While GI histoplasmosis may involve any portion of the GI tract, nearly 90% of lesions involve the lower GI tract, most commonly the ileocecal region or colon.
1-4 In the largest case series of GIH in AIDS patients, duodenal disease was appreciated in <4% of cases, making it one of the rarest sites of GI involvement.
4 Treatment with antifungal agents is recommended for most cases of disseminated histoplasmosis. Mild to moderate disease should be treated with oral itraconazole 200 mg twice a day, leading to response rates of 80-100%. For severe disease, treatment with amphotericin B for 2 weeks followed by oral itraconazole 200 mg twice a day is recommended. The standard duration for treatment is at least 12 months.
2,4,5 It must be emphasized that, although the etiology of duodenal ulcer may take some time to be figured out, treatment for the acute bleeding in histoplasmosis is the same as usual and specific therapy only initiates after histological examination.
Conclusion
Although this represents a rare cause of GI bleeding, it should be considered when immunocompromised subjects present acute hemorrhage. Early recognition, diagnosis, and treatment of GI histoplasmosis in high-risk populations prior to these events would probably improve patient outcomes.
References
- Chu JH, Feudtner C, Heydon K, Walsh TJ, Zaoutis TE. Hospitalizations for endemic mycoses: a population-based national study. Clin Infect Dis. 2006;42(6):822-5.
- Kauffman CA. Histoplasmosis. Clin Chest Med. 2009;30(2):217-25.
- Spinner MA, Paulin HN, Wester CW. Duodenal histoplasmosis presenting with upper gastrointestinal bleeding in an AIDS patient. Case Rep Gastrointest Med. 2012;2012:515872.
- Lim SY, Kijsirichareanchai K, Winn R. Progressive disseminated histoplasmosis in systemic lupus erythematosus: an unusual presentation of acute tenosynovitis and a literature review. Clin Rheumatol. 2013;32(1):135-9.
- Weng CT, Lee NY, Liu MF, et al. A retrospective study of catastrophic invasive fungal infections in patients with systemic lupus erythematosus from southern Taiwan. Lupus. 2010;19(10):1204-9.