48uep6bbphidcol2|ID
48uep6bbphidvals|1756
48uep6bbph|2000F98CTab_Articles|Fulltext
Peliosis hepatis is a rare lesion which, on histology, shows blood filled dilated sinusoids or cystic spaces. It can be seen with hepatocellular carcinoma (HCC), hepatic adenoma (HA), and mostly reported following intake of medication, especially oral contraceptives, androgen, anabolic steroids and azathioprine. HCC showing peliosis hepatis with dilatation of sinusoids, mimicking cavernous hemangioma has seldom been reported.
1,2 Early irregular enhancement of the peripheral part of the mass lesion on magnetic resonance imaging (MRI) and on arteriography, mimics characteristic features of a cavernous haemangioma making differentiation between the two lesions impossible on imaging. We report this rare lesion in a 63-year- old man which on radiology showed a large mass lesion with features of hemangioma and was later diagnosed to be a case of well differentiated hepatocellular carcinoma (WD-HCC) with peliotic change on histopathology.
Case Report
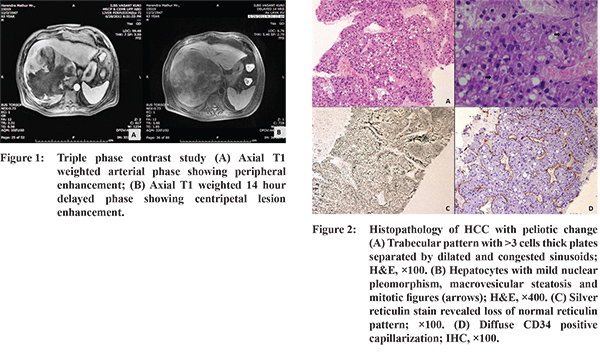
63-year-old male, was admitted in the department of Hepatology with the complaints of weakness and loss of appetite for 3 months. On examination he had tender hepatomegaly, 4 cms below the right costal margin. Laboratory investigations showed normal complete blood count except for low hemoglobin of 9.3 gm/dl. His liver function tests showed total bilirubin of 3.2 mg/dl with direct fraction of 1.6mg/dl, aspartate aminotransferase (AST) was 185 IU/L, alanine aminotransferase (ALT) was 85 IU/L, serum alkaline phosphatase (SAP) was 118 IU/L, gamma glutamyl transferase (GGT) was 94 IU/L, total protein of 6.5 gm/dl with albumin of 2.2 gm/dl and INR of 1.4. Viral markers and serology for Hepatitis A, B, C and HIV were negative. There was no history of alcohol or drug intake. His serum alpha-fetoprotein (AFP) was 72.33 ng/ml and protein induced by vitamin K antagonist II (PIVKA II) was 179.35 ng/ml. These raised levels of AFP and PIVKA II raised the suspicion for the possibility of a malignant lesion. MRI abdomen showed a large, rounded, well defined mass of 15.8x15.6 cm, displaying heterogeneous signal intensity with mixed hyper and hypo-intense signal on T1 weighted and T2 weighted images. On triple phase contrast study, the lesion showed peripheral nodular enhancement in arterial phase (Figure 1A) with centripetal filling in portal venous phase and delayed images (Figure 1B). On imaging, a diagnosis of giant cavernous hemangioma was made. However, in view of raised AFP and PIVKA II the clinical differential also included HCC and therefore, USG guided fine needle aspiration cytology (FNAC) was requested. On FNAC, diagnosis of hemangioma was ruled out. Few thick trabeculae of mildly atypical hepatocytes were seen on the FNA. Tru-cut liver biopsy was advised to rule out the possibility of HCC. Histopathological examination of the liver biopsy showed distortion of the lobular architecture with markedly dilated and congested sinusoids. The portal tracts and central veins (hepatic veins) were absent. Hepatocytes formed thickened cell plate and trabeculae of 4-7 cell thickness, separated by dilated and congested sinusoids (Figure 2A). These thickened trabeculae comprised of hepatocytes with mild nuclear pleomorphism and fair amount of cytoplasm with macrovesicular steatosis. Few mitotic figures were also seen (Figure 2B). Silver reticulin stain revealed poor or absent staining in the tumour areas (Figure 2C). Immunohistochemical (IHC) studies were done. There was diffuse CD34 positive capillarization (Figure 2D). MIB labelling index was approx 8%. In view of the histomorphological features and their confirmation by histochemical stains (HC) and IHC, the diagnosis of WD-HCC with peliosislike areas was confirmed. Later, a PET-CT done, revealed a well marginated periphery and avid FDG uptake in the heterogeneously enhancing hypodense lesion in the right lobe of liver. The patient was planned for three sittings of transarterial chemoembolization with doxorubicin eluting beads. The patient received the first sitting of chemotherapy and has been on regular follow-up.
Discussion
WD-HCC with peliotic change is a rare histological diagnosis. Peliotic hepatitisis seen in patients with a history of oral contraceptive use or steroid intake. However, in the absence of drug history, peliosis is extremely rare. A few cases have been reported with wasting diseases like tuberculosis and AIDS.
3 Peliotic areas have been described in the liver tissue surrounding HCC in autopsy cases. Peliotic change is usually observed in moderately or poorly differentiated type of HCC.
3 However, peliosis in a WD-HCC mass itself is seldom reported.
3-5 In a recent study by Nomura et al, out of 1225 patients of HCC, only seven cases showed WD-HCC with peliotic change.
5 All the reported cases including our case were elderly males. Contrary to our case, which had no underlying viral etiology, the case reported by Kim et al
4 was Hepatitis B antigen positive andthe case reported by Hoshimoto et al3 and Ji et al1 was positive for hepatitis C virus antibody,. Resembling our findings, the study by Nomura et al described five cases that were negative for viral markers.
5 Another case reported by Kawasaki et al showed Technetium-99m red blood cell (RBC) scintigraphy findings in a case of peliotic HCC mimicking hemangiomathough pathological confirmation could not be obtained.
2 On radiology, the findings of peliosis hepatis are variable and it often mimics hemangioma. The dynamic CT or MRI findings of classical HCC are quite diagnostic with hyperattenuation in the hepatic arterial phase and isoattenuation or hypoattenuation in the portal venous and delayed phases. However, HCC with peliotic change shows early peripheral enhancement in arterial phase as a bright rim with progressive central filling in portal venous phase and delayed phase as in cavernous hemangioma.
2-4 This is because, in this variant of HCC, multiple, large,pelioid spaces might have been responsible for the gradual fill-in enhancement pattern as in cavernous hemangioma, and the intervening thick trabeculae of HCC may be the cause of scattered areas of low attenuation in the enhancing portions. The possible mechanism to the formation of peliosis could be the blockade of outflow of blood from the liver at the hepatic sinusoid-venule junction.
3,5 In cases like ours, it is very difficult to differentiate between cavernous hemangioma and HCC with peliosis on imaging alone and therefore liver biopsy is the gold standard.
The main differential diagnosis on histological examination is between well differentiated HCC with peliosis and telangiectatic adenoma. Both lesions show dilated sinusoids and increase in cell plate thickness. However, the features which favour HCC include cell plate thickness of more than three cells, reticulin poor areas and capillarization on CD34 staining. Other soft points which may help are nuclear hyperchromasia and nuclear membrane irregularity, presence of mitotic figures and high MIB labelling index, all of which favour the diagnosis of HCC.
References
- Ji EK, Ryu JS, Kang GH, Moon DH, Auh YH, Lee HK. Pelioid type hepatocellular carcinoma masquerading as a hepatic hemangioma on technetium-99m red blood cell scintigraphy. Clin Nucl Med. 2001;26:33-5.
- Kawasaki T, Kudo M, Inui K, Ogawa C, Chung H, Minami Y. Hepatocellular carcinoma mimicking cavernous hemangioma on angiography and contrast enhanced harmonic ultrasonography. A case report. Hepatol Res. 2003;25:202-12.
- Hoshimoto S, Morise Z, Suzuki K, Tanahashi Y, Ikeda M, Kagawa T, Mizoguchi Y, Sugioka A. Hepatocellular carcinoma with extensive peliotic change. J Hepatobiliary Pancreat Surg. 2009;16(4):566-70.
- Kim YK, Jang KY, Cho BH, Ko SW, Moon WS. Three-phase dynamic CT of pelioid hepatocellular carcinoma. Am J Roentgenol. 2007;189:160-2.
- Nomura Y, Nakashima O, Kumabe T, Akiba J, Ogasawara S, Kage M, Kinoshita H,Yano H. Clinicopathologic analysis of the simple nodular type of well-differentiated hepatocellular carcinoma with extensive peliotic change. J Gastroenterol Hepatol. 2014;29(7):1494-99.