48uep6bbphidcol2|ID
48uep6bbphidvals|1718
48uep6bbph|2000F98CTab_Articles|Fulltext
Incidence of skull metastasis has been reported to vary from 15-25%.
1 The primary sites being most commonly breast, lung, prostate, thyroid and kidney. Metastasis from hepatocellular carcinoma (HCC) to the skull is very rare with an incidence of 0.5-1.6%.
2-4 We report case of an elderly male who presented with a scalp swelling whichwas finally diagnosed as a metastatic deposit of HCC.
Case Report
A 70 year-old male presented with a right sided scalp swelling for previous 1 year which was gradually increasing in size along with progressive loss of vision for 6 months. There was no history of loss of consciousness, neurological deficit, significant weight loss or loss of appetite. He had one episode of jaundice 7 years ago for which he was hospitalized for 1 week.
On examination, a swelling measuring 15x10x5 cm was present over right temporo-parietal region and extending till lateral canthus of right eye and inferiorly to upper border of right ear. The complete blood count, kidney function tests and thyroid function tests were within normal limits. However, liver function tests were mildly deranged with serum bilirubin=2mg/dl, indirect bilirubin=1.3mg/dl, AST=99U/l & ALT=49U/l.
Cranial radiogram showed a lytic lesion involving both inner & outer table. Chest radiogram and ECG were within normal limits. Contrast enhanced computerized tomography (CECT) showed a large enhancing lesion arising from right parietal and temporal bone with extension into right temporo-parieto-frontal region, right orbital cavity and overlying scalp tissue. CECT abdomen and chest was performed which revealed a lesion measuring 8x6x5 cm in segment IVB & III of liver which was possibly metastatic along with metastatic deposits in T1, T2 & T3 vertebral bodies and in right superior pubic ramus.
Fine needle aspiration (FNA) was performed at multiple sites of the scalp swelling. The smears were highly cellular with presence of variably sized loosely cohesive sheets and clusters of cells with occasional glandular patterns closely associated with capillaries. The individual cells were large with moderate to abundant cytoplasm with presence of intracytoplasmic dark pigment in many cells. (Figure 1)
The nuclei were round with vesicular chromatin and prominent nucleoli and few exhibited intranuclear inclusions and occasionally nuclear grooving. A diagnosis of metastatic carcinoma to the scalp was considered with possibilities of primary from thyroid carcinoma, renal cell carcinoma (RCC), HCC, lung adenocarcinoma, adrenocortical carcinoma (ACC), prostatic adeno carcinoma and malignant melanoma. Repeated ultrasound guided FNA cytology from thyroid yielded no tissue only blood.
Trucut biopsy was performed on the scalp swelling. It showed tumor tissue with cells arranged in a predominantly glandular pattern. The glands were separated by fine vascular spaces. The individual cells were large with abundant clear to eosinophilic cytoplasm, moderate anisonucleosis with vesicular chromatin and prominent nucleoli. Few cells showed presence of intracytoplasmic brown pigment. There were numerous mitotic figures. Occasional cell revealed intranuclear cytoplamic inclusions. (Figure 2) Cell cytoplasm stained positively with PAS. Masson’s Fontana stain for melanin and Perl’s stain for iron were negative.
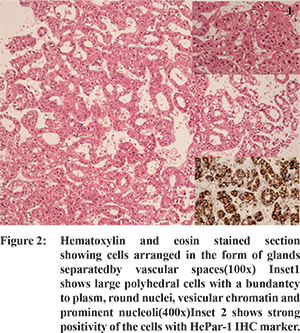
Immunohistochemistry (IHC) was performed.Tumor cells showed strong positivity for pancytokeratin (CK) while they were negative for cytokeratin 7 (CK7), cytokeratin 20 (CK20) and vimentin. However, vimentin was positive in the vascular spaces in between the cells. The negative result on CK7,CK20 helped rule out transitional cell carcinoma, pancreatic adenocarcinoma, lung adenocarcinoma, gastric adenocarcinoma and colorectaladeno carcinoma. HMB 45 and thyroglobulin were negative ruling out malignant melanoma and follicular/papillary carcinoma of the thyroid respectively. The differential diagnosis of CK positive, CK7 negative and CK 20 negative tumors includes RCC, HCC, ACC and prostatic adeno carcinoma. Epithelial membrane antigen (EMA) and CD 10 were tested subsequently; EMA was negative ruling out ACC which was further confirmed by inhibin negativity. CD 10 was positive thus narrowing down the diagnosis to metastasis from RCC, HCC and prostatic adeno carcinoma. RCC antigen and PSA were negative ruling out RCC and prostatic adeno carcinoma respectively. Hep Par 1 was strongly positive (Figure 2) and thus the nature of the metastatic deposit was confirmed to be HCC.
Cytology smears were reviewed and there were presence of few macrotrabeculae, acinar spaces and clusters showing transgressing blood vessels. However, there was no definite endothelial wrapping. The greenish black pigment was bile.
Discussion
Skull metastasis from HCC is found to usually affect males in their sixth and seventh decades
5 as found in the present case. Metastasis from HCC to the central nervous system generally occurs through two different pathways. The first is the osseous route via the Bateson’s venous plexus to the skull (osteophilic cancer) as was seen in the current case. The other is the hematogenous route via the lung to the brain parenchyma without involvement of the skull (neurophilic cancer).
This article emphasizes the fact that although cytology can help in differentiating between benign and malignant lesions, IHC is indispensible in making a definitive diagnosis.
References
- Bradley WG, Daroff RB, Fenichel GM, Jankovic J. Neurology in clinical practice. 4th ed. Philadelphia: Elsevier. 2004. vol 2 p. 1455.
- Chan CH, Trost N, McKelvieP, Rophael JA, Murphy MA. Unusual case of skull metastasis from hepatocellular carcinoma. ANZ J Surg. 2004;74:710-713.
- McIver JI, Scheithauer BW, Rydberg CH, Atkinson JL: Metastatic hepatocellular carcinoma presenting as epidural hematoma: case report. Neurosurgery. 2001;49:447-449.
- Shim YS, Ahn JY, Cho JH, Lee KS. Solitary skull metastasis as initial manifestation of hepatocellular carcinoma. World J of Surg Oncol. 2008;6:66.
- Ellyda MN, MohdShafie A. Solitary skull metastasis as initial manifestation of Hepatocellular Carcinoma - A case report. The International Medical Journal. 2009;8(2):47-51.