|
|
|
|
 |
 |
| |
 |
|
|
Original Articles |
|
|
|
|
|
Keywords :
Hemobilia, hemetemesis, obstructive jaundice, embolisation, endovascular approach |
|
|
TV Prasad1, AK Gupta1, P Garg2, S Pal3, S Gamanagatti1
Department of Radiodiagnosis1,
Gastroenterology2 and
Gastrointestinal Surgery3
All India Institute of Medical Sciences,
New Delhi-110029
Corresponding Author:
Dr Shivanand Gamanagatti
Email: shiv223@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.280
Abstract
Hemobilia is a well known cause for upper gastrointestinal (UGI) bleed seen commonly in setting of iatrogenic or accidental trauma and various inflammatory and neoplastic conditions. Patients present with UGI bleed and symptoms of associated biliary obstruction. Management options in intractable cases are surgery and endovascular embolisation. We report a series of eighteen patients presented with severe hemobilia from January 2010 to October 2014, who were managed by endovascular approach in our department. Etiology in these patients were trauma (n=3), liver biopsy (n=3), surgery (n=3), percutaneous procedures (n=2), inflammatory (n-3), neoplasm (n=1) and the rest were idiopathic. Angiography revealed pseudoaneurysms of hepatic artery (n=5), splenic artery (n=1) and gastroduodenal artery (n=1) and arteriobiliary fistula (n=1). Embolising agents used were detachable coils (n=10) and glue (n=8). All patients had technical and clinical success with minor non-consequential complications. Our findings show that endovascular embolisation is a simple, safe, accurate and effective treatment in patients with severe hemobilia. It is a viable alternative to major and potentially morbid surgeries.
|
48uep6bbphidvals|1344 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext Hemobilia, defined as bleeding within or into the biliary tree, has been a recognized cause of massive upper gastrointestinal hemorrhage (UGIH) from early seventeenth century.[1] The patients present with symptoms of biliary obstruction and UGIH in varying severity. Hemobilia has to be considered in the differential diagnosis when UGIH is associated with biliary symptoms. Hemobilia is often seen as a complication of inflammatory disorders, percutaneous and surgical hepatobiliary interventions, trauma and rarely neoplasms. The management algorithm in these patients is depended on the basic disease process, severity of bleeding and hemodynamic condition of the patient at presentation. It includes surgical and endovascular methods when conservative measures fail. Here we present a series of patients with hemobilia who were managed in our department by endovascular approach.
Materials and methods
Patient population
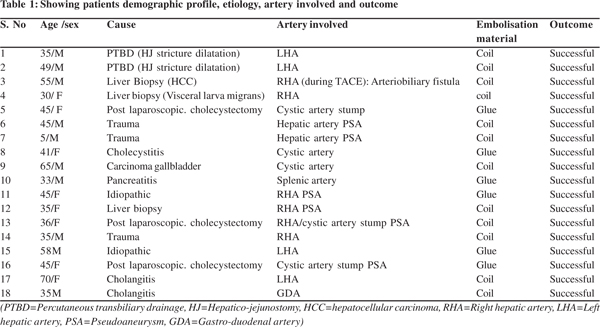
From January 2010 to October 2014 we encountered eighteen patients presenting with hemobilia. Ten were male and eight were female with a median age of 43 yrs. Three patients had prior history of blunt abdominal trauma wi th liver injury. Three patients developed hemobilia as a complication of liver biopsy procedure among which one patient each had hepatocellular carcinoma and visceral larva migrans. In three patients, inadvertent injury to vessels during laparoscopic cholecystectomy was the cause. Two patients developed hemobilia following percutaneous transbiliary procedure for hepatico-jejunostomy stricture. Rest of the patients had acute cholangitis (n=2), acute cholecystitis (n=1), acute pancreatitis (n=1) and carcinoma gall bladder (n=1) as the inciting cause. In two patients no known risk factors could be identified. (Table 1). Common clinical presentations include upper gastrointestinal hemorrhage, abdominal pain and obstructive jaundice. Three patients presented with unstable hemodynamic status following massive hemetemesis.
Procedures
Cross sectional imaging
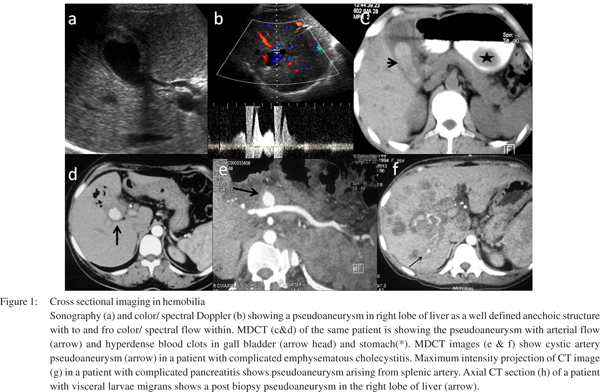
Ultrasonography (USG) was performed in few patients who presented to emergency with chief complaints of abdominal pain. Multi detector computed tomography (MDCT) was offered to selected patients depending upon the hemodynamic status of the patient and renal parameters. MDCT accurately detect bleeding vessels and pseudoaneurysms in most of the patients and gave a road map in angiography procedures (Figure 1).
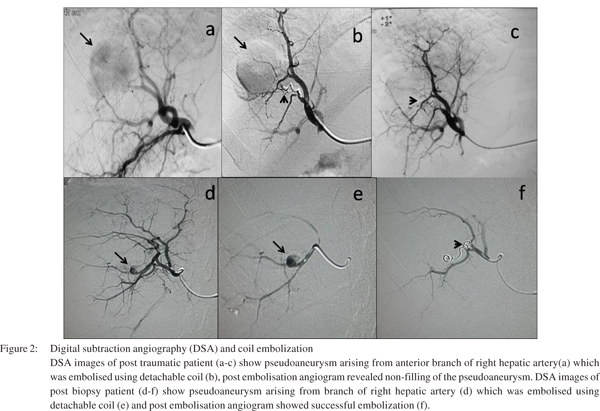
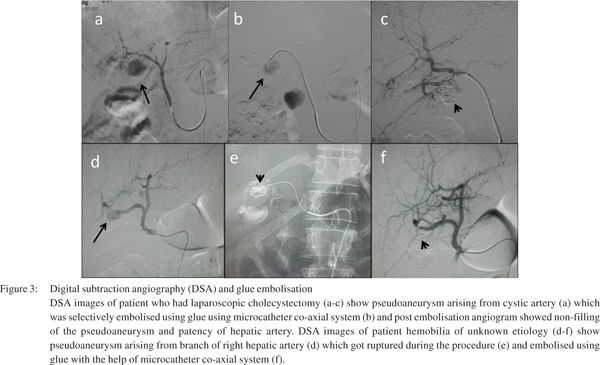
Digital subtraction angiography (DSA) was performed in all the patients. Diagnostic angiography revealed pseudoaneurysms in hepatic artery branches/ cystic artery (n=15), splenic artery (n=1) and gastroduodenal artery (n=1). One patient had arteriobiliary fistula. Celiac arteries were catheterized using 5F RC1 (Boston Scientific, Natick, Massachusetts) catheters. Superselective cannulation of the culprit vessels was done prior to therapeutic embolisation. Microcatheters (Progreat 2.7 F microcatheter, Terumo; Terumo Corporation, Tokyo, Japan) were used in selective cases. For ten patients with pseudoaneurysms and one with arterio-biliary fistula detachable stainless steel coil was used as embolising agent (Figure 2). In rest of the patients the aneurysms were obliterated using glue (liquid agent, n-butyl-2-cyanoacrylate (NBCA), 30-50% NBCA-Lipiodol combination) (Figure 3). Blockage of neck of pseudoaneurysms and hence their complete thrombosis was ensured in all the cases.
Results
MDCT was performed in eleven patients prior to angiography. It revealed pseudoaneurysms arising from various vessels (hepatic arteries, cystic artery, splenic artery) as given in Table 1. In one patient arterio-biliary fistula was diagnosed during TACE (transarterial chemoembolisation) procedure for hepatocellular carcinoma. Angiographic procedures were technically successful in all the patients. Bleeding was arrested in all the patients and all of them showed clinical improvement.
Most of the patients complained of transient abdominal pain following the procedure which got resolved with analgesics and conservative measures. On three month follow up all the patients were doing well. In our study, two patients had nontarget embolisation of glue particles into the hepatic parenchyma, but did not develop any major consequences related to this complication.
Discussion
The term hemobilia was coined by Sandblom in 1948.[2] Since then, several reports of hemobilia can be found in literature. It is an unusual cause of UGIH which occurs due to an abnormal vascular communication with biliary tree. Various inflammatory disorders of hepato-biliary system can be complicated with hemobilia. It should also be suspected in any patient with history of recent or remote liver trauma or instrumentation presenting with UGIH. The site of bleeding can be intra or extrahepatic biliary tract, gall bladder, pancreatic duct or the ampulla of Vater. The severity of hemobilia depends on the type of pathological process, the vessel involved and nature of vascular lesion. Most of the patients in literature had history of either accidental or iatrogenic trauma prior to the presentation.[3-5] In majority of our patients previous abdominal trauma and surgery were the leading cause. The patients are often evaluated with endoscopy, sonography (USG), computed tomography (CT), magnetic resonance imaging (MRI) and angiography. Endoscopy is primary modality in patients presenting with UGIH. In our series, six patients underwent endoscopy as the first investigation. In hemodynamically stable patients a cross sectional modality (USG, CT or MRI angiography) is done to assess the basic pathology and site of bleeding. Subsequent management involves resuscitation, arrest of bleeding and relieving biliary obstruction. The treatment options are conservative approach, surgery and angiographic embolisation.
Conservative approach is feasible only in cases of low grade bleeding in patients with normal hemodynamic status. Surgery is often difficult in these cases because of extensive adhesions and edema because most of these patients have in the clinical settings of prior surgery, trauma or active inflammation. There are increasing evidence in the literature in the use of selective angioembolisation as an important method to address the patients with hemobilia.[6–10] Angiography is a minimally invasive procedure combining the advantages of diagnosis and treatment. It can avoid major risky surgical procedures having high morbidity. The common vascular pathologies detected at angiography are pseudoaneurysms and arteriobiliary fistulas. Bilio-venous fistulas rarely cause significant hemobilia and they are usually managed by conservative measures, biliary catheter repositioning or biliary stenting.
The common embolising agents used in the past were detachable coils, gel foams and glue. In our series we used either coils or glue as the embolising agent. Embolisation Coils: These are permanent mechanical embolising agent (EA), available in variable configurations. Small fibers attached to metal component illicit thrombogenic response, leading to vascular occlusion. Adequate scaffolding obtained by initially deploying a larger coil followed by smaller ones and can be used as a scaffold in combination with Gelfoam; such a ‘‘coil-Gelfoam sandwich’’ causes a complete, permanent mechanical occlusion. For selection of coil size, as a rule of thumb, coil size should be 20% larger than vessels diameter (approximately one size more than diameter of vessel).
Cyanoacrylate (Glue): It is a liquid embolising agent has property of tissue adhesive. Polymerizes rapidly once exposed to ionic environment and incites inflammatory reaction, forms a cast and vessel occlusion. Ethiodol mixture ratio is used to modulate the polymerization time per operator’s preference (1:1– 1:6), with higher concentrations of lipiodol conferring prolonged polymerization times. Disadvantages of use of glue, requires expertise, catheter can become entrapped in the occluded vessel. Polymerization can spread distally or reflux proximally leading to non-target embolisation.
Gelfoam: Biodegradable temporary EA, derived from subcutaneous porcine adipose tissue. It is available as a block of sponge or as a powder and can be used as slurry when mixed with contrast. Gelfoam torpedoes or cubes may also be used for larger vessels. Recanalization of the vessel can occur within 3 weeks- 3 months. Most commonly used embolising agent is coil, which is the best embolising agent in this situation. However, choice of embolising agent may vary from case to case basis, depending upon size of vessel, type of vessel, expertise and availability of hardwares.
Choice of embolising agent in specific situations
If the culprit vessel is end artery and can be reached super selectively, choice of embolising agent is coil. In some situations, even after coil embolisation, flow to pseudoaneurysm is reduced but not completely occluded. In such situation, the embolising effect is further supplemented by either glue or gelfoam as sandwich technique. If the pseudoaneurysm is arising from main/major artery like common hepatic artery, isolation of pseudoaneurysm from the main artery is ideal way of treating this kind of pseudoaneurysm. Choice is either stent graft or filling the pseudoaneurysm sac with glue. Occasional the bleeder is in the form of abnormal blush or the bleeder could not be reached because of tortuosity of vessel. In such cases, just gelfoam embolisation may help in achieving hemostasis.
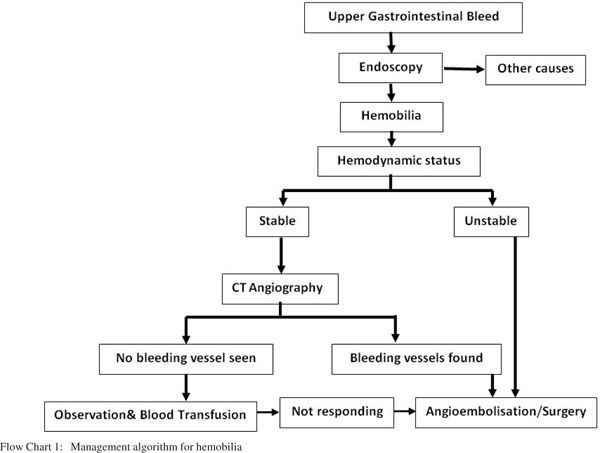
In our study complications observed were transient abdominal pain and fever which were resolved by conservative measures. Other serious complications reported in literature are hepatic necrosis, hepatic failure, non-target embolisation and sepsis. Superselective catheterization of bleeding vessels combined with optimal selection of embolising agents and their careful deployment can decrease the frequency of complications. A treatment algorithm followed in our institute is given (Flow chart 1).
Although angiography is the most useful diagnostic and therapeutic modality, it may not be successful in all the cases. The focus of bleeding may be angiographically obscure when bleeding is intermittent. Moreover procedure can be difficult with anomalous, tortuous or atherosclerotic vessels or previously ligated vessels. MDCT angiography prior to the procedure will help in these cases to localize the bleeding and to find alternate vascular routes.
In conclusion, selective angioembolisation is a safe, minimally invasive and effective procedure which can be performed routinely for the patients presenting with hemobilia. It has an excellent success rate with proper planning and careful deployment of optimal embolising agents. Detachable coils and glue are safe embolizing agents when deployed after superselective catheterisation with negligible complication rates.
References
- Glisson F. Anatomia Hepatis, 1st Edition. Amsterdam, Janssonium and Weyerstraten, 1654.
- Sandblom P. Hemorrhage into the biliary tract following trauma; traumatic hemobilia. Surgery. 1948;24:571–86.
- Green MH, Duell RM, Johnson CD, Jamieson NV. Haemobilia. Br J Surg. 2001;88:773–86.
- Merrell SW, Schneider PD. Hemobilia—evolution of current diagnosis and treatment. West J Med. 1991;155:621–5.
- Caminiti R, Rossitto M, Ciccolo A. Pseudoaneurysm of the hepatic artery and hemobilia: a rare complication of laparoscopic cholecystectomy; clinical case and literature review. Acta Chir Belg. 2011;111:400–3.
- Srivastava DN, Sharma S, Pal S, Thulkar S, Seith A, Bandhu S, et al. Transcatheter arterial embolization in the management of hemobilia. Abdom Imaging. 2006;31:439–48.
- Perlberger RR. Control of hemobilia by angiographic embolization. AJR Am J Roentgenol. 1977;128:672–3.
- Nicholson T, Travis S, Ettles D, Dyet J, Sedman P, Wedgewood K, et al. Hepatic artery angiography and embolization for hemobilia following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol. 1999;22:20–4.
- Hidalgo F, Narváez JA, Reñé M, Domínguez J, Sancho C, Montanyà X. Treatment of hemobilia with selective hepatic artery embolization. J Vasc Interv Radiol JVIR. 1995;6:793–8.
- Lee M, Himal HS. Hemobilia—successful treatment by angiographic embolization. Surg Endosc. 1992;6:75–7.
|
|
|
 |
|
|