M. Rojas-Feria1, M. Eslam1, M. Castro-Fernandez1, Eva Leon-Jimenez 2, Manuel Romero-Gomez1
Unit for The Clinical Management of Digestive Diseases and CIBERehd1,
Unit of Infectious Disease, and CIBERehd,2
Hospital Universitario de Valme,
Ctra de Cadiz s/n, Sevilla 41014, Spain.
Corresponding Author:
Dr. Maria Rojas-Feria,
Email: mrojasferia@yahoo.es
DOI:
http://dx.doi.org/10.7869/tg.2012.77
48uep6bbphidvals|562 48uep6bbph|2000F98CTab_Articles|Fulltext Invasive aspergillosis is a devastating disease, associated with high morbidity and mortality.Primary infection usually involves the respiratory tract following environmental exposure to aspergillus and in severely immunocompromised patients, it disseminates to other organs.[1]
Case report
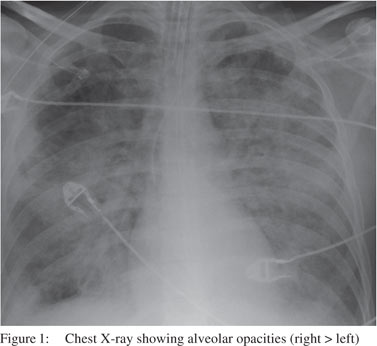
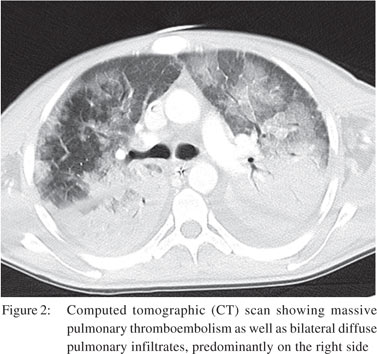
A 24 year old male smoker diagnosed with ileocecal Crohn’s disease in July 2010, initially required intravenous corticosteroids to achieve remission. But in August 2010, the patient was admitted with right iliac pain which was nonresponsive to oral corticosteroids. He was subsequently treated with intravenous methylprednisolone - 1 mg/kg/day and azathioprine - 2.5 mg/kg/day. Levels of thiopurine methyltransferase were normal. The patient improved and was discharged on oral mesalazine 3 g once daily, azathioprine and gradual tapering of corticosteroids. Two months later, he was readmitted with another outbreak of activity that required intravenous corticosteroids, however, on day 10, he developed marked neutropenia. He complained of cough with purulent sputum, wheeze and dysnea but there was no chest pain or haemoptysis. On examination, he was found to have low grade fever with scattered coarse crepitations. Chest X-ray revealed alveolar opacities (right more than left) without any large pleural effusion, discrete mass, or nodules (Figure 1). Computed tomographic (CT) scan showed massive pulmonary thromboembolism as well as bilateral diffuse pulmonary infiltrates, predominantly on the right side (Figure 2).
Bronchoscopy showed white covering histologically corresponding to invasive aspergillosis, with detection of aspergillus specific antigen (galactomannan) in bronchoalveolar lavage and respiratory secretions. After obtaining blood and sputum cultures, empirical intravenous broad-spectrum antibiotics and antifungal agents were started immediately. Azathioprine was immediately withdrawn, with rapid tapering of corticosteroid, till complete stoppage. Later, blood, sputum and bronchoalveolar lavage cultures revealed light growth of aspergillus species. The patient initially received antifungal therapy with voriconazole plus caspofungin, then was subsequently maintained on voriconazole monotherapy for four months. Owing to the drug interaction between oral anticoagulation and voriconazole, patient was maintained on subcutaneous heparin for anticoagulation. In addition, he was put on mesalazine 3 g every day. Serial follow up of serum aspergillus galactomannan antigen was negative and radiological evaluation (serial chest X-ray) showed modest improvement, repeat sputum culture tests were negative and multiple blood culture tests were negative. Though his ICU stay was prolonged, there was marked clinical and radiological improvement at the time of discharge.
 Discussion
Patients with IBD may be at risk of developing aspergillus lung infections.[2] Unfortunately, serious infections including life-threatening opportunistic infections, following exposure to immunosuppressive regimens is a well-known problem. The risk for acquisition of these infections following exposure of tumour necrosis factor alpha (TNFa) antibody therapies including infliximab and adalimumab has been demonstrated in series of cases.[3] However, it is critical to direct the attention that the risk of opportunistic infection is also present in those who are receiving other immunosuppressive therapy rather than the biological therapies. Our patient had concurrent treatment with prednisone when azathioprine was initiated.
Discussion
Patients with IBD may be at risk of developing aspergillus lung infections.[2] Unfortunately, serious infections including life-threatening opportunistic infections, following exposure to immunosuppressive regimens is a well-known problem. The risk for acquisition of these infections following exposure of tumour necrosis factor alpha (TNFa) antibody therapies including infliximab and adalimumab has been demonstrated in series of cases.[3] However, it is critical to direct the attention that the risk of opportunistic infection is also present in those who are receiving other immunosuppressive therapy rather than the biological therapies. Our patient had concurrent treatment with prednisone when azathioprine was initiated.
Albeit, the threshold levels for risk of serious infections with steroid therapy have not been clearly delineated, one study of patients receiving corticosteroids after renal transplantation found that a daily dose of prednisone equal to or greater than 1.25 mg/kg was a risk factor for aspergillosis.[4]
References
- Segal BH. Aspergillosis. N Engl J Med. 2009;360:1870–84.
- Casella G, Villanacci V, Di Bella C, Antonelli E, Baldini V, Bassotti G. Pulmonary diseases associated with inflammatory bowel diseases. J Crohns Colitis. 2010;4:384–9.
- Manz M, Beglinger C, Vavricka SR. Fatal invasive pulmonary aspergillosis associated with adalimumab therapy. Gut. 2009;58:149.
- Gustafson TL, Schaffner W, Lavely GB, Stratton CW, Johnson HK, Hutcheson RH Jr. Invasive aspergillosis in renal transplant recipients: correlation with corticosteroid therapy. J Infect Dis. 1983;148:230–8.
|