|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
R Agrawal1, S Mittal2, M Jain3, GS Lamba3
Departments of General Surgery,1
Medicine2 and Gastroenterology,3
Maharaja Agarsen Hospital,
Punjabi Bagh, New Delhi, India.
Corresponding Author:
Dr. Rati Agrawal
Email: drrati_agr@yahoo.com
DOI:
http://dx.doi.org/10.7869/tg.2012.61
48uep6bbphidvals|546 48uep6bbph|2000F98CTab_Articles|Fulltext In the Indian subcontinent, ascariasis is highly endemic in Kashmir (70%), Bangladesh (82%), and central and southwest India (20-49%).[1] We report here a case of acute pancreatitis following ascariasis within the main pancreatic duct.
Case report
A 24-year-old female presented to our Emergency Department with high grade fever and moderate, non-colicky right hypochondrial pain, associated with vomiting since 2 days. The patient was icteric, had tender hepatomegaly and liver function tests showed a serum bilirubin of 2.4 mg% and AST of 11,740 IU/ml and ALT of 7220 IU/ml. IgM anti HAV was positive and a diagnosis of acute viral hepatitis A was made. After 5 days of conservative management, the patient improved symptomatically and was discharged from the hospital. But she returned one day after her discharge with severe boring continuous abdominal pain in the epigastric region which was radiating to the back and was associated with vomiting. Abdominal examination revealed marked epigastric tenderness and repeat liver function tests showed a serum bilirubin of 8.4 mg% , AST: 168 IU/ml, ALT: 793 IU/ml. Serum amylase was 1346 IU/ml and serum lipase was 2249 U/L.
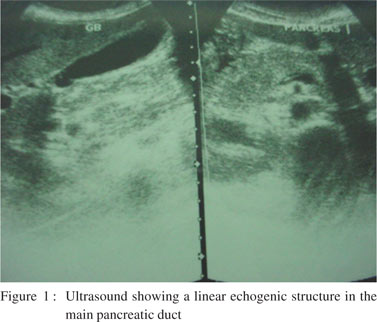
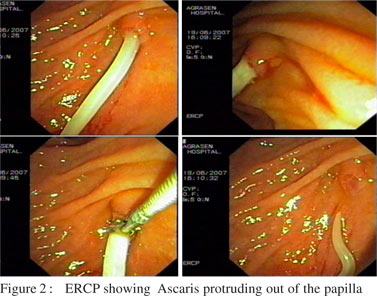
A clinical diagnosis of acute pancreatitis was made and the patient was kept on conservative management. Ultrasound (Figure 1) examination revealed hepatomegaly, an edematous gall bladder, normal common bile duct (CBD) and hypoechoic bulky pancreas more towards the tail region, with a linear echogenic structure in the main pancreatic duct extending from the region of the head of pancreas up to the tail. The ‘fourlines sign’ was distinguishable on scanning the duct in cross section. However the patient’s condition did not improve and the next day a contrast enhanced CT scan of abdomen was performed, which showed an enlarged pancreas with decreased attenuation, shaggy outline with ill-defined peripancreatic planes and peripancreatic fluid suggestive of acute edematous pancreatitis. The pancreatic duct was dilated (3 mm in diameter), in the region of the pancreatic head and body. A curvilinear tubular soft tissue attenuation filling defect was seen in contrast opacified duodenum extending up to the ampulla of Vater with an air speck within, possibly a round worm infiltrating the ampulla (USG correlation was also done). An MRCP showed a mildly dilated main pancreatic duct (3 mm in diameter) harboring a hypointense linear structure with surrounding hyperintensity in proximal part of the main pancreatic duct. The same day after the MRCP, the patient underwent an ERCP (endoscopic retrograde cholangiopancreatography, (Figure 2) in which an Ascaris protruding out of the papilla was seen. The round worm was grasped with a foreign body forceps, and retrieved from the papilla and the body. There was dramatic relief in pain and the patient’s general condition improved. Oral feed was started and the patient was discharged four days after ERCP and removal of the worm.
 Discussion
The adult worm can invade the biliary or pancreatic ducts, or both, and cause complications such as biliary duct obstruction, cholecystitis, cholangitis and acute pancreatitis. Invasion of the pancreatic duct is rare because of its narrow caliber.[2] A case of a 64-year-old lady with acute pancreatitis was reported by Price et al[3] in 1988, in which pancreatic duct ascariasis was diagnosed based on the characteristic ultrasonographic appearance known as the “four-lines” sign.
Khuroo et al[4] in his report on hepatobiliary and pancreatic ascariasis in India, examined 500 patients out of which 64 patients presented with acute cholecystitis, 121 with acute cholangitis, 280 with biliary colic, four with hepatic abscess and 31 with pancreatitis. The worms were found in various locations including 274 patients having it in their duodenum, 171 patients in the biliary tree, 40 patients in the hepatic channel, eight patients in the gall bladder and seven patients in the pancreatic duct. Phylogenic cholangitis occurred in 27 patients out of which two needed surgical drainage and the remaining 25 improved after ERCP drainage. The worm was removed in 280 patients. Four patients succumbed to their condition including, two due to pancreatitis, one due to cholangitis and one due to hepatic abscess. Reinvasion was noted in 76 patients. Sandouk et al[5] published their experience of 300 patients from Syria and showed that ultrasonography, together with clinical findings, are the mainstay of diagnosing pancreatic ascariasis.
References
Discussion
The adult worm can invade the biliary or pancreatic ducts, or both, and cause complications such as biliary duct obstruction, cholecystitis, cholangitis and acute pancreatitis. Invasion of the pancreatic duct is rare because of its narrow caliber.[2] A case of a 64-year-old lady with acute pancreatitis was reported by Price et al[3] in 1988, in which pancreatic duct ascariasis was diagnosed based on the characteristic ultrasonographic appearance known as the “four-lines” sign.
Khuroo et al[4] in his report on hepatobiliary and pancreatic ascariasis in India, examined 500 patients out of which 64 patients presented with acute cholecystitis, 121 with acute cholangitis, 280 with biliary colic, four with hepatic abscess and 31 with pancreatitis. The worms were found in various locations including 274 patients having it in their duodenum, 171 patients in the biliary tree, 40 patients in the hepatic channel, eight patients in the gall bladder and seven patients in the pancreatic duct. Phylogenic cholangitis occurred in 27 patients out of which two needed surgical drainage and the remaining 25 improved after ERCP drainage. The worm was removed in 280 patients. Four patients succumbed to their condition including, two due to pancreatitis, one due to cholangitis and one due to hepatic abscess. Reinvasion was noted in 76 patients. Sandouk et al[5] published their experience of 300 patients from Syria and showed that ultrasonography, together with clinical findings, are the mainstay of diagnosing pancreatic ascariasis.
References
- Khuroo MS. Hepatobiliary and pancreatic ascariasis. Indian J Gastroenterol. 2001;20:C28–32.
- Agarwal A, Chowdhary V, Srivastava N, Khera G, Singh S. Pancreatic duct ascaris: sonographic diagnosis—a case report. Trop Gastroenterol. 2005;26:197–8.
- Price J, Leung J.W.C.Ultrasound diagnosis of Ascaris lumbricoides in the pancreatic duct:the “four-lines”sign. Br J Radiol. 1988;61:411–3.
- Khuroo MS, Zargar SA, Mahajan R. Hepatobiliary and pancreatic ascariasis in India. Lancet. 1990;335:1503–6.
- Sandouk F, Haffar S, Zada MM, Graham DY, Anand BS. Pancreatic-biliary ascaris: experience of 300 cases. Am J Gastroenterol. 1997;92:2264–7.
|
|
|
 |
|
|