|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Ashish Kumar Jha, Sandeep Nijhawan, Rupesh Pokharna, Subhash Nepalia, Arya Suchismita
Department of Gastroenterology,
SMS Medical College, Jaipur, India
Corresponding Author:
Dr. Ashish Kumar Jha
Email: ashishjhabn@yahoo.co.in
DOI:
http://dx.doi.org/10.7869/tg.2012.62
48uep6bbphidvals|547 48uep6bbph|2000F98CTab_Articles|Fulltext Discussion
There is a widespread use of mesh for abdominal wall hernia repair. Migration of mesh could occur soon after surgery or many years later, even after twenty years of hernioplasty.[1]
The use of polypropylene meshes (PP mesh) for abdominal wall hernia repair is common and its complications are being increasingly recognized. Delayed migration of mesh is a rare and difficult to diagnose condition because of variable clinical presentations. Migration of mesh into a hollow viscous leading to a colo-cutaneous fistula (CCF) has rarely been reported. We present a case of delayed migration of PP mesh and subsequent CCF formation which was diagnosed by colonoscopy after seven years of open left lumbar hernia repair.
Case report
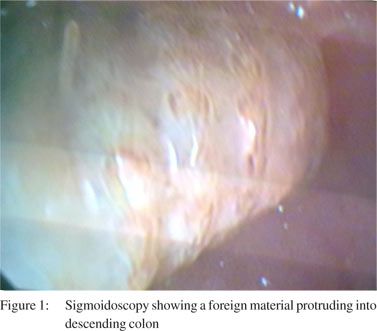
A 48-year-old male presented with two months history of feculent discharge from left abdominal flank , low grade fever and abdominal pain. He gave history of open left lumbar hernia (acquired type) repair and mesh implantation 7 years back. A fistulous opening with indurated margins was seen in the left lumbar region. Mild tenderness was present over the left hypochondrium. Bowel sounds were normal. Laboratory investigations revealed a hemoglobin of 10.5 gm/dl with normal erythrocytes and a total leukocyte count of 18,000/mm3 with 85% polymorphonuclear leukocytes. Blood sugar, renal and liver function tests were normal. Abdominal plain radiographs were normal. Abdominal computed tomography (CT) revealed pericolonic stranding (descending colon) with a soft tissue tract extending through the oblique and rectus muscles, and subcutaneous and cutaneous regions, suggestive of a CCF. Sigmoidoscopy revealed a foreign material protruding into the colon at 30 cm from the anal verge (Figure 1). This material was neither movable nor extractable by endoscopic snare. The patient was placed on broad spectrum antibiotics and other supportive measures. Surgical exploration revealed adhesions of the large bowel with the mesh and associated scarring. A fistulous tract extending from the descending colon to the left lumbar region was noted and a PP mesh was found embedded in the descending colon. Removal of the mesh along with resection of the affected bowel segment followed by an anastomosis was performed. The patient is doing well at sixmonth follow-up.
 Discussion
Discussion
There is a widespread use of mesh for abdominal wall hernia repair. Migration of mesh could occur soon after surgery or many years later, even after twenty years of hernioplasty.[1]
Mesh migration may have varied presentations depending on the organ involved. Most reported cases in the literature involve the urinary bladder. Intraluminal migration into a hollow viscous is rare.[2] Clinical manifestations of mesh migration into the intestine are variable and can present as abdominal pain, intraabdominal abscess, intestinal obstruction, intestinal perforation, intermittent diarrhoea, haematochezia and fistulae.[3-7] It can even mimic diverticulitis.[8] Detection of a migrated mesh is very difficult. In plain film radiographs neither the PP nor the expanded polytetraûuorethylene mesh (e-PTFE mesh) are visible. Ultrasound is a useful method for identifying meshes, but it has several limitations. CT scan seems to offer better mesh visualization, but failure to detect migrated PP mesh by CT scans is also common.[9-11] Owing to their different compositions and thickness, the PP and the e-PTFE mesh have different appearances on a CT scan. The PP meshes are visible as lines with a density similar to the adjacent muscles in only 20% of patients however, the e-PTFE mesh appears as a line of increased density visible in all patients.[16] Colonoscopy is the single best investigation for the detection of a mesh which has migrated into the large bowel.[7,8] In our patient the migrated mesh missed by CT was detected by colonoscopy, supporting the observation that CT is a poor modality for such diagnosis.
References
- Weitzel SH, Botha AJ, Thomas PA. Late colocutaneous fistula after mesh repair of an inguinal hernia. Hernia.1998;2:39–40.
- Agrawal A, Avill R. Mesh migration following repair of inguinal hernia: a case report and review of literature. Hernia. 2006;10:79–82
- Miller K, Junger W. Ileocutaneous fistula formation following laparoscopic polypropylene mesh hernia repair. Surg Endosc. 1997;11:772–3.
- Goswami R, Babor M, Ojo A. Mesh erosion into caecum following laparoscopic repair of inguinal hernia (TAPP): a case report and literature review. J Laparoendosc Adv Surg Tech A. 2007;17:669–72.
- Ferrone R, Scarone PC, Natalini G. Late complication of open inguinal hernia repair: Small bowel obstruction caused by intraperitoneal mesh migration. Hernia. 2003;7:161–2.
- Losanoff JE, Richman BW, Jones JW. Entero-colocutaneous fistula: a late consequence of polypropylene mesh abdominal wall repair: case report and review of the literature. Hernia. 2002;6:144–7.
- Lange B, Langer C, Markus PM, Becker H. Mesh penetration of the sigmoid colon following transabdominal preperitoneal hernia repair. Surg Endosc. 2003;17:157.
- El Hakam MZ, Sharara AI, Chedid V. Persistent left lower abdominal pain: Mesh migration into the sigmoid Colon. Gastroenterol. 2010;138:e5–6
- Ott V, Groebli Y, Schneider R. Late intestinal fistula formation after incisional hernia using intraperitoneal mesh. Hernia. 2005;9:103–04.
- de Hoyos A, Villegas O, Sanchez JM, Monroy M A. Endoloops as a therapeutic option in colocutaneous fistula closure. Endoscopy. 2005;37:1258.
- Parra JA, Revuelta S, Gallego T, Bueno J, Berrio JI, Farinas MC. Prosthetic mesh used for inguinal and ventral hernia repair: Normal appearance and complications in ultrasound and CT. Br J of Radiol. 2004;77:261–5.
|
|
|
 |
|
|