|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Malay Sharma, AlShumrany MA, Pazhanivel Mohan
Department of Gastroenterology,1
Jaswant Rai Specialty Hospital, Meerut, India
Corresponding Author:
Dr. Malay Sharma
Email: sharmamalay@hotmail.com
DOI:
http://dx.doi.org/10.7869/tg.2012.15
48uep6bbphidvals|500 48uep6bbph|2000F98CTab_Articles|Fulltext Biliary “sump syndrome” is an infrequent complication of sideto- side choledochoduodenostomy (CDD) performed for achieving permanent drainage of common bile duct (CBD). It is associated with recurrent stone formation in about 40% due to the stenosis of CDD and failure of the dilated CBD to decompress after CDD. Endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy (ES) is regarded as the treatment of choice for sump syndrome but has a restenosis rate as high as 19%, necessitating repeat papillotomy. We report a case of sump syndrome successfully managed by dilatation of the stenosed CDD using an upper GI endoscope.
Case report
Biliary “sump syndrome” is an infrequent complication of sideto- side choledochoduodenostomy (CDD) performed for achieving permanent drainage of common bile duct (CBD).[1]
It is associated with recurrent stone formation in about 40% due to the stenosis of CDD and failure of the dilated CBD to decompress after CDD.[2,3] Endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy (ES) is regarded as the treatment of choice for sump syndrome but has a restenosis rate as high as 19%, necessitating repeat papillotomy.[4,5]
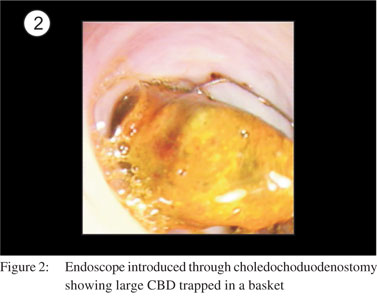
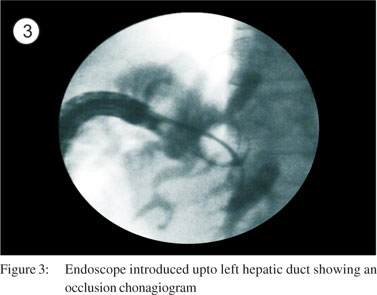
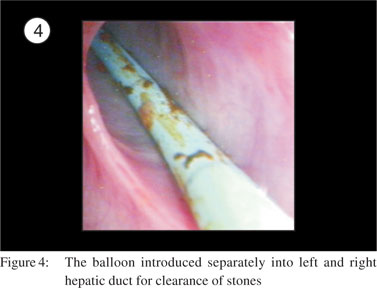
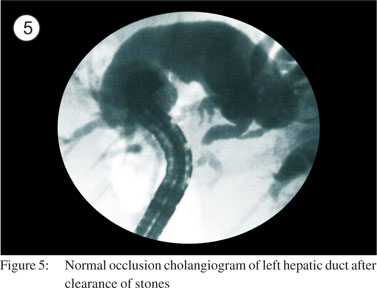
A 60-year-old man presented with a history of recurrent cholangitis. He underwent cholecystectomy and side-to-side CDD 10 years back and an ERCP three years back for retained CBD stone due to sump syndrome. Ultrasound abdomen revealed a massively dilated CBD with multiple CBD stones and a repeat ERCP was planned. Side viewing scopy failed to show the ampulla but the opening of a partially blocked CDD was seen. The cholangiogram through CDD confirmed the presence of multiple large stones (Figure 1). The opening of CDD was dilated by putting a CRE balloon (microvasive-TTS balloon, 15-18 mm diameter, 240 cm length) through an UGI endoscope. After dilatation of CDD the UGI endoscope was negotiated into the biliary tree for removal of stones under vision (Figure 2). The larger fragments were removed by basket and smaller fragments of stones lying in dependent part of the left intrahepatic bile duct were cleared by passing a balloon with the help of a terumo wire (0.032mm) into distal most part of both the ducts (Figures 3 and 4). The clearance of the biliary tract was confirmed by an occlusion cholangiogram as well as direct visualization using the UGI endoscope (Figures 5 and 6)

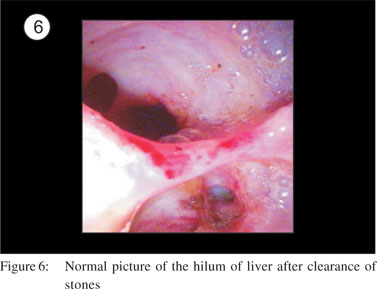
This case demonstrates that recurrent stones after CDD can be successfully managed by dilatation of the stenosed CDD and clearance of stones under direct vision using an upper GI endoscope.
References
- Ueno N, Ozawa Y, Aizawa T. Prognostic factors for recurrence of bile duct stones after endoscopic treatment by sphincter dilation. Gastrointest Endosc. 2003;58:336-40.
- Keizman D, Shalom MI, Konikoff FM. An angulated common bile duct predisposes to recurrent symptomatic bile duct stones after endoscopic stone extraction Surg Endosc. 2006; 20:1594-9.
- Kibria SM, Hall R. Recurrent bile duct stones after transduodenal sphincteroplasty. HPB (Oxford). 2002;4:63-6.
- Rizzutti, RP, McElwee TB, Carter JW. Choledochoduodenostomy. A safe and efficacious alternative in the treatment of biliary tract disease. Am Surg. 1987; 53:22–5.
- Caroli-Bosc FX, Demarquay JF, Peten EP, Dumas R, Bourgeon A, Rampal P, et al. Endoscopic management of sump syndrome after choledochoduodenostomy: retrospective analysis of 30 cases. Gastrointest Endosc. 2000; 51 :180-3.
|
|
|
 |
|
|