Sijil Kottikkal Sivaraman, Premaletha Sunil, K.R.V. Kumar
Department of Medical Gastroenterology,
Medical College, Thiruvananthapuram, India
Corresponding Author:
Dr. Sijil kottikkal sivaraman
Email: drsijil@gmail.com
48uep6bbphidvals|734 48uep6bbph|2000F98CTab_Articles|Fulltext Case report
A 43-year-old lady without associated comorbidity presented with upper abdominal dull aching pain, persistent nonbilious vomiting,loss of appetite and loss of weight.Clinical examination revealed pallor. Routine diagnostic work up revealed iron deficiency anemia. The endoscopic examination of the stomach showed thickened rugal folds and nondistensible stomach.Endoscopic biopsy was non informative.
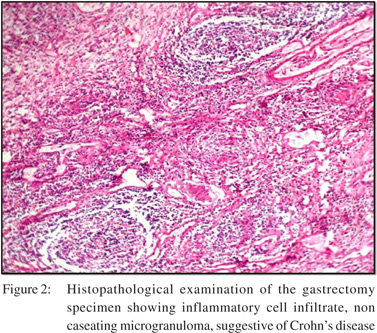
CECT abdomen showed evidence of thickened stomach with perigastric small lymph nodes.The patient had undergone gastrectomy in view of gastric outlet symptoms and had significant anorexia and weight loss.Gastrectomy specimen showed diffusely thickened stomach with macroscopic appearance of linitis plastica (Figure 1).Histopathology examination revealed transmural inflammatory cell infiltrate, and microgranulomas suggestive of Crohn’s disease (Figure 2).

The patient was diagnosed as Crohn’s disease and further workup revealed multiple strictures in the small bowel though large bowel was normal and subsequently managed with azathioprine and supportive medications.
Discussion
Gastric Crohn’s is a rare condition.Most of the patients are asymptomatic and if symptomatic, they present either with upper abdominal pain with postprandial aggravation,[1]or with symptoms suggestive of gastric outlet obstruction (persistent vomiting) due to stricture formation. Anemia may be a feature due to chronic blood loss. The gold standard investigation to diagnose gastric Crohn’s is endoscopic biopsy.[2] The usual endoscopic findings are focal gastritis appearing as erythema, mucosal friability, thickened folds, and ulcerations.
Characteristic endoscopic finding is mucosal nodularity.[3] Some patients may show evidence of diffuse gastric involvement with endoscopic resemblance tolinitis plastica.[4] The histological examination may reveal noncaseating granuloma. The most common finding in histopathological examination is focal inflammatory cell infiltrate suggesting focal gastritis.[5] Gastric Crohn’s may be treated symptomatically in the initial stages.Steroids to induce remission followed by azathioprine or mercaptopurine may be used in patients with severe disease. Infliximab hasnot been widely studied in isolated gastric crohns disease.[6]
References
- Nugent FW, Roy MA. Duodenal Crohn’s disease: an analysis of 89 cases. Am J Gastroenterol.1989;84:249–54.
- Reynolds HL, Jr, Stellate TA. Crohn’s disease of the foregut. Surg Clin North Am. 2001;81:117–35.
- Wagtmans MJ, van Hogezand RA, Griffioen G, Verspaget HW, Lamers CB. Crohn’s disease of the upper gastrointestinal tract. Neth J Med. 1997;50:S2–S7.
- Fenoglio-Preiser CM, Noffsinger AE, Stemmermann ON, Lantz PE, Listrom MB, Rilke FO.Gastrointestinal Pathology. 2nd ed. Philadelphia: Lippincott-Raven; 1999. The nonneoplastic stomach; pp. 153–236.
- Loftus EV Jr. Upper gastrointestinal tract Crohn’s disease. Clin Perspect Gastroenterol. 2002;5:188–91.
- Valori RM, Cockel R. Omeprazole for duodenal ulceration in Crohn’s disease. BMJ. 1990;300:438–9.
|