Murat Özgur Kilic1, Gurkan Degirmenciioglu1, Cenap Dener1, Nur Arslan2
Department of General Surgery1 and Pathology2,
Faculty of Medicine, Turgut Özal University,
Ankara, Turkey
Corresponding Author:
Dr. Murat Özgür KILIÇ
Email: murat05ozgur@hotmail.com
48uep6bbphidvals|726 48uep6bbph|2000F98CTab_Articles|Fulltext Colorectalcancer (CRC) is the third most frequently diagnosed cancer in both men and women and the second most fatal cancer.[1] The incidence of CRC is greater in men than in women.[2] CRCs are often seen in the elderly population and approximately 30% of these are localized in the rectum.[2] Distal rectal cancer is a surgical and oncological challenge. Various surgical operations, such as abdomin operineal resection and low anterior resection with total mesorectal excision (TME), are performed in the management of distal rectal cancer. Although recurrence rates have decreased to about 10% after using the method of TME, local recurrence remains an important clinical issue.[3] Surgery is the treatment of choice but it is a difficult procedure, with very poor prognosis. Here, we report a case of pelvic recurrent tumor that was entirely excised by a novel and alternative surgical method, transperineal approach, with CTguided wire marking.
Case Report
A 71-year-old female patient, who had undergone abdominal operineal resection for a low rectal cancer with T2N0 pathological stage before fifteen months, was admitted to our unit for routine follow-up. She had received a full course of adjuvant chemoradiation following the operation. On blood tests, cancer antigen 19.9 (CA 19-9) level was high (163 IU/mL) with normal carcinoembryonic antigen (CEA) level (5ng/mL).
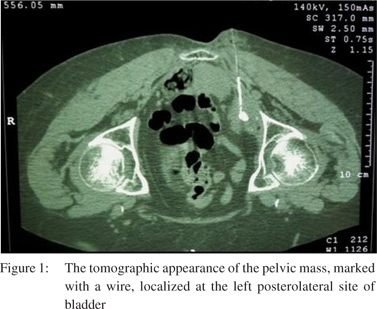
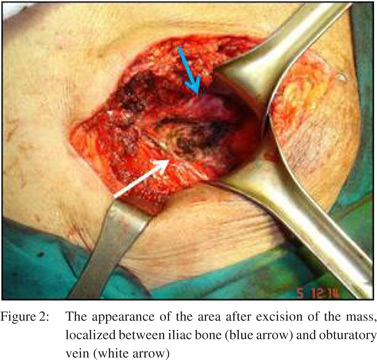
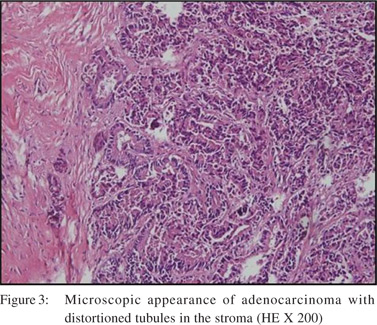
As shown in Figure 1, CT scan showed a heterogeneous pelvic mass, 38 mm x 35 mm in size, at the left posterolateral side of bladder. Similar lesion within definite borders was also seen on magnetic resonance imaging. In PET/CT, an increased 18F - FDG uptake (SUVmaks: 5.1), approximately 29 mm x 25 mm in size, at the inferior left para-iliac zone was observed. CTguided trucut biopsy was performed. Biopsy identified an adenocarcinoma. The pelvic mass was marked with a CT-guided wire and was excised totally by transperineal approach under spinal anesthesia as shown in Figure 2. On histopathological examination, an adenocarcinoma, evaluated as a recurrent lesion of the primary rectal cancer, was reported as shown in Figure 3.
Discussion
The most important component for obtaining long term local control and survival is R0 resection with sharp TME. Additionally, the use of adjuvant radiotherapy has been shown to reduce loco-regional recurrence (LR).[4] However, patients, treated with a curative rectal cancer resection, have a 10% risk of developing LR.[3] Close anatomic relation of the rectum to the small pelvis makes rectal cancer proneto recurrence. LR of rectal cancer usually occurs within the first few years following resection of the primary.[5] Similarly, the pelvic recurrence developed fifteen months after primary surgery in our case.
The stage of primary tumor and a positive circumferential resection margin infers an LR risk and poor prognosis.[6] Rates of LR or distant metastases are 5 - 10% in stage A, but 40-70% in stage C.[7] Our patient had a T2N0 tumor with clear radial margins and no perforation occurred during the surgery. In addition, the patient had adjuvant radiotherapy and chemotherapy. As is well known, the CEA level is a useful marker for follow-up of colorectal cancer recurrence. In our patient, the CEA level was normal but CA 19.9 level was increased. Morales-Gutierrez et al also showed in their study that elevated level of CA 19.9 was an independent risk factor for recurrence and was associated with a poor prognosis.[8] The surgical treatment of LR is particularly challenging, however patients with LR have a median survival of approximately 8 months without treatment.[9] The 5-year overall survival rate after the operation for LR is approximately 50% even where surgery is possible.[10] Unfortunately, only a small proportion of patients with LR have a chance of surgery. These patients are usually operated via laparotomy ortransanally. But these methods have their own limitations. In selected patients, the transperineal approach may be the most easy and appropriate way for resection of recurrent pelvic lesions. Thus, the difficulties of laparotomy are avoided. However, adequate preoperative radiological evaluation must be done. In addition, marking the lesion is very helpful for the success of the operation in a transperineal approach. As far as we know, this is the first case of rectal cancer recurrence treated via the transperineal approach. Finally, LR is a major cause of morbidity and mortality in patients undergoing curative resection of rectal cancer. Surgical resection is the recommended treatment modality and can be performed safely by the transperineal approach in selected patients.
References
- Siegel R, Naishadham D, Jemal A.Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
- Rim SH, Seeff L, Ahmed F, King JB, Coughlin SS. Cancer Colorectal cancer incidence in the United States, 1999–2004: an updated analysis of data from the National Program of Cancer Registries and the Surveillance, Epidemiology, and End Results Program. 2009;115:1967–76.
- Das P, Skibber JM, Rodriguez-Bigas MA, Feig BW, Chang GJ, Hoff PM, et al. Clinical and pathologic predictors of locoregional recurrence, distant metastasis, and overall survival in patients treated with chemoradiation and mesorectal excision for rectal cancer. Am J Clin Oncol. 2006;29:219–24.
- Nissan A, Guillem JG, Paty PB, Douglas Wong W, Minsky B, Saltz L, et al. Abdominoperineal resection for rectal cancer at a specialty center. Dis Colon Rectum. 2001;44:27–35
- Davies M, Harris D, Hirst G, Beynon R, Morgan AR, Carr ND, et al. Local recurrence after abdomino-perineal resection. Colorectal Dis. 2009;11:39–43.
- Kelly SB, Mills SJ, Bradburn DM, Ratcliffe AA, Borowski DW; Northern Region Colorectal Cancer Audit Group. Effect of the circumferential resection margin on survival following rectal cancer surgery. Br J Surg. 2011;98:573–81.
- Burdy G, Panis Y, Alves A, Nemeth J, Lavergne-Slove A, Valleur P. Identifying patients with T3-T4 node negative colon cancer at high risk of recurrence. Dis Colon Rectum. 2001;44:1682–8.
- Morales-Gutierrez C, Vegh I, Colina F, Gomez-Camara A, IgnacioLanda J, Ballesteros D, et al. Survival of patients with colorectal carcinoma: possible prognostic value of tissular carbohydrate antigen 19.9 determination. Cancer. 1999;86:1675–81.
- Moriya Y. Treatment strategy for locally recurrent rectal cancer. Jpn J Clin Oncol. 2006;36:127–31.
- Tanaka K, Noura S, Ohue M, Seki Y, Yamada T, Miyashiro I, et al. Doubling time of carcinoembryonic antigen is a significant prognostic factor after the surgical resection of locally recurrent rectal cancer. Dig Surg. 2008;25:319–24.
|