Bivas Biswas1, Atul Sharma1, Govind K Makharia2, Sanjay Thulkar3, Sudheer Arava4, Ankur Bahl1, Surendra Chaudhary1
Departments of Medical Oncology1, Gastroenterology 2,
Radiodiagnosis3 and Pathology,4
Dr. B. R. A. Institute Rotary Cancer Hospital, All India Institute of Medical Sciences
Ansari Nagar, New Delhi - 110029, India
Corresponding Author:
Dr. Atul Sharma
Email: atul1@hotmail.com
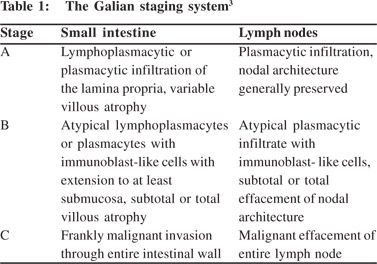
48uep6bbphidvals|691 48uep6bbph|2000F98CTab_Articles|Fulltext Immunoproliferative small intestinal disease (IPSID) is a rare low-grade B-cell lymphoma arising from mucosa associated lymphoid tissue (MALT), representing approximately one-third of intestinal lymphoma. Histopathologically it is characterized by infiltration of small bowel wall with lymphocytes and plasma cells. The infiltrates produces an aberrant immunoglobulin (IgA), a truncated alpha heavy chain without the light chain component.[1,2] Galian et al[3] described the disease in three stages depending upon type of cellular infiltrate and mesenteric nodal involvement (Table 1). Presentation may mimic that of celiac disease, tropical sprue or parasitic infestation and patients are being treated on the line of celiac disease and other causes of malabsorption for prolonged duration before being diagnosed as IPSID/NHL.[4,5] Emaciation and diarrhoea is due to malabsorption syndrome and protein losing enteropathy secondary to lymphoma infiltration of intestine. Most patients present during early stages and are curable with oral antimicrobials.6 Few may progress to high-grade lymphoma requiring systemic chemotherapy. We present here the clinico-pathological characteristics, treatment and outcome of six patients treated at our institute during the last 10 years, along with a review of literature.
Case reports
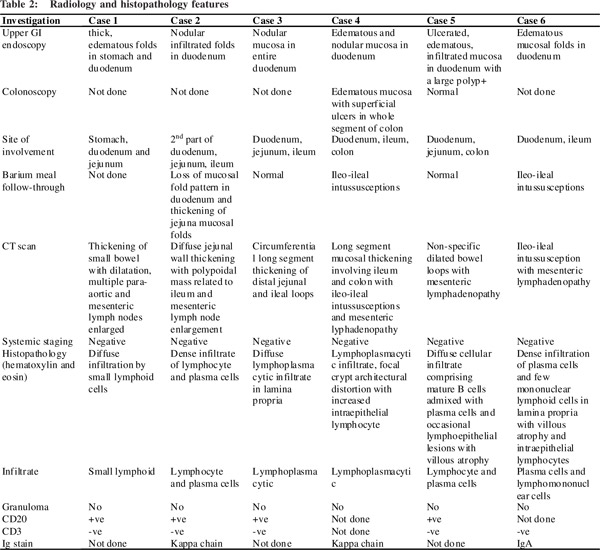
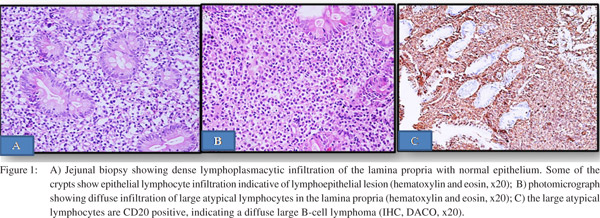
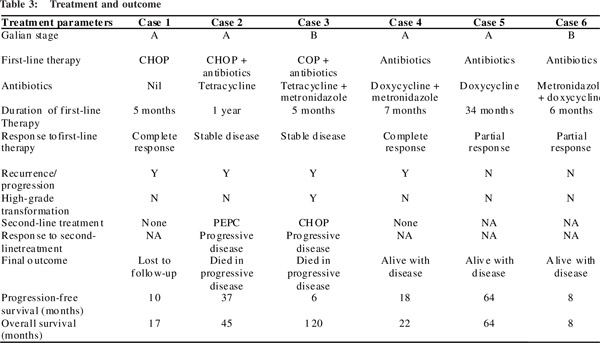
A total of six patients with median age of 27 years (range: 15- 35) were identified and treated. Median duration of symptom was 13.5 months (range: 6-26). All patients presented with history of recurrent watery loose motion with decreased appetite, weight loss and low grade fever. The median time from diagnosis of malabsorption to diagnosis of IPSID was 10 months (range: 1–20). Test for alpha heavy chain protein (AHCP) in serum was not done. Barium meal follow through showed ileo-ileal intussusception in case number 4 and 6 (Table 2). All patients showed evidence of oedematous mucosal thickening in small bowel and enlarged mesenteric lymph nodes on CT scan. Endoscopic biopsy of mucosal lesions showed diffuse infiltrate of small atypical lymphoid cells or lymphoplasmacytic cells (Figure 1A) which were CD20+CD3- with partial or total villous atrophy. Repeat biopsy during progression showed features of high grade B-cell lymphoma in case number 3 (Figures 1B & 1C). Galian stage, treatment details and outcome are summarised in Table 3. Case number 1 received 6 cycles of CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) and achieved complete response (CR) lasting for 10 months and then was lost to follow-up. Case 2 also received 6 cycles of CHOP with tetracycline (1g/day) and was in stable condition for 1 year after which the disease progressed, and the patient succumbed 45 months after initial diagnosis of IPSID. Case 3 initially received CVP (cyclophosphamide, vincristine, and prednisolone) along with oral metronidazole and tetracycline (MT) without any response. Repeat biopsy revealed a high-grade B- non-Hodgkin’s lymphoma (NHL). He was given 6 cycles of CHOP but his disease continued to progress. He eventually succumbed 120 months after diagnosis of IPSID. Case 4 achieved CR after MT lasting for 14 months. Currently she is asymptomatic and on regular follow-up. Case 5 achieved partial remission after oral doxycycline and is continuing on regular follow-up with same treatment. The last patient was diagnosed recently and is on doxycycline and metronidazole. Though the sample size is too small for survival analysis, we calculated a median progressionfree survival of 18 months and overall survival of 64 months after a median follow-up of 22 months.
 Discussion
The infectious aetiology of IPSID has been supported by the demonstration of H. pylori and C. jejuni in tumor samples of IPSID.[7,8] Al-Saleem et al[9] reported the largest series comprising of 89 IPSID patients out of a total 145 cases of small intestinal lymphoma. There are few published reports from India as well.[4,5,10] Presentation of our cases was similar to published literature; including chronic diarrhoea, abdominal pain, weight loss, low-grade fever and clubbing.[9,11–13] Very few patients in literature with a diagnosis of chronic malabsorption syndrome have been reported as IPSID.[14–16] The exact pathogenesis of IPSID is unknown. Pathologically it shows a spectrum of disease with alpha-HCD (with AHCP production), with Mediterranean lymphoma on one hand and frank high-grade malignant lymphoma on the other. AHCP is present in approximately 87% of patients with IPSID.[17] If left untreated the disease may progress to high-grade malignant lymphoma.
Clinical staging depends on type of cellular infiltrate, severity of involvement and lymph node histopathology. Galian staging is most commonly used and classifies the disease into three stages (A, B and C).
Discussion
The infectious aetiology of IPSID has been supported by the demonstration of H. pylori and C. jejuni in tumor samples of IPSID.[7,8] Al-Saleem et al[9] reported the largest series comprising of 89 IPSID patients out of a total 145 cases of small intestinal lymphoma. There are few published reports from India as well.[4,5,10] Presentation of our cases was similar to published literature; including chronic diarrhoea, abdominal pain, weight loss, low-grade fever and clubbing.[9,11–13] Very few patients in literature with a diagnosis of chronic malabsorption syndrome have been reported as IPSID.[14–16] The exact pathogenesis of IPSID is unknown. Pathologically it shows a spectrum of disease with alpha-HCD (with AHCP production), with Mediterranean lymphoma on one hand and frank high-grade malignant lymphoma on the other. AHCP is present in approximately 87% of patients with IPSID.[17] If left untreated the disease may progress to high-grade malignant lymphoma.
Clinical staging depends on type of cellular infiltrate, severity of involvement and lymph node histopathology. Galian staging is most commonly used and classifies the disease into three stages (A, B and C).
The clinical course is indolent in IPSID. Though very responsive to antibiotics in early stages, the disease can progress to high-grade lymphoma if left untreated. It can cause severe morbidity secondary to malabsorption and protein losing enteropathy. Early treatment is important to control the disease and malabsorption and prevent its progression.[13] In a retrospective study of 21 Tunisian patients with IPSID, 6 had early stage disease and responded well to antibiotics. [15] patients with high/intermediate grade disease were treated with an anthracycline containing combination chemotherapy (CHOP/or CHOP-like). The overall remission rate was 90±12% at 2 years and 67±25% at 3 years.[18] In first 2 patients we employed anthracycline-based chemotherapy given our lack of experience. Another large Turkish study also reported similar results[19] Rambaud et al[13] recommended antibiotic treatment for early stage and CHOP for those with inadequate response to oral antibiotics and for advanced stage disease. The optimum duration for antibiotics is not known, and perhaps might be required lifelong. The role of surgery is limited and is used only for symptom palliation and rarely for salvage. The usual cause of death is disease progression or transformation to high-grade lymphoma and complications of malnutrition. In our study, all six patients showed early response to antibiotics but ultimately three patients suffered disease progression. Two patients died of progressive disease; one underwent transformation to high-grade B-cell lymphoma, while remaining three patients are doing well on treatment.
References
- Seligmann M, Danon F, Hurez D, Mihaesco E, Preud’homme JL. Alpha-chain disease: a new immunoglobulin abnormality. Science. 1968;162:1396–7.
- Isaacson P, Wright DH. Malignant lymphoma of mucosaassociated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983;52:1410–6.
- Galian A, Lecestre MJ, Scotto J, Bognel C, Matuchansky C, Rambaud JC. Pathological study of alpha-chain disease, with special emphasis on evolution. Cancer. 1977;39:2081–101.
- Ghoshal UC, Chetri K, Banerjee PK, Choudhuri G, Pal BB, Dabadghao S, et al. Is immunoproliferative small intestinal disease uncommon in India? Trop Gastroenterol. 2001;22:14–7.
- Puri AS, Kumar M, Khan EM, Pandey R, Aggarwal R, Naik S, et al. Immunoproliferative small intestinal disease: a frequently missed diagnosis. Indian J Gastroenterol. 1996;15:46–8.
- Fine KD, Stone MJ. Alpha-heavy chain disease, Mediterranean lymphoma, and immunoproliferative small intestinal disease: a review of clinicopathological features, pathogenesis, and differential diagnosis. Am J Gastroenterol. 1999;94:1139–52.
- Fischbach W, Tacke W, Greiner A, Konrad H, Muller H. Regression of immunoproliferative small intestinal disease after eradication of Helicobacter pylori. Lancet. 1997;349:31–2.
- Lecuit M, Abachin E, Martin A, Poyart C, Pochart P, Suarez F, et al. Immunoproliferative small intestinal disease associated with Campylobacter jejuni. N Engl J Med. 2004;350:239–48.
- Al-Saleem T, Zardawi IM. Primary lymphomas of the small intestine in Iraq: a pathological study of 145 cases. Histopathology. 1979;3:89–106.
- Nair S, Mathan M, Ramakrishna BS, Mathan VI. Immunoproliferative small intestinal disease in South India: a clinical and immunomorphological study. J Gastroenterol Hepatol. 1998;13:1207–11.
- Salem P, Anaissie E, Allam C, Geha S, Hashimi L, Ibrahim N, et al. Non-Hodgkin’s lymphomas in the Middle East. A study of 417 patients with emphasis on special features. Cancer. 1986;58:1162–6.
- Al-Saleem T, Al-Mondhiry H. Immunoproliferative small intestinal disease (IPSID): a model for mature B-cell neoplasms. Blood. 2005;105:2274–80.
- Rambaud JC, Halphen M, Galian A, Tsapis A. Immunoproliferative small intestinal disease (IPSID): relationships with alpha-chain disease and “Mediterranean” lymphomas. Springer Semin Immunopathol. 1990;12:239–50.
- Yadav P, Das P, Mirdha BR, Gupta SD, Bhatnagar S, Pandey RM, et al. Current spectrum of malabsorption syndrome in adults in India. Indian J Gastroenterol. 2011;30:22–8.
- Ranjan P, Ghoshal UC, Aggarwal R, Pandey R, Misra A, Naik S, et al. Etiological spectrum of sporadic malabsorption syndrome in northern Indian adults at a tertiary hospital. Indian J Gastroenterol. 2004;23:94–8.
- Ghoshal UC, Mehrotra M, Kumar S, Ghoshal U, Krishnani N, Misra A, et al. Spectrum of malabsorption syndrome among adults & factors differentiating celiac disease & tropical malabsorption. Indian J Med Res. 2012;136:451–9.
- Salem PA, Estephan FF. Immunoproliferative small intestinal disease: current concepts. Cancer J. 2005;11:374–82.
- Ben-Ayed F, Halphen M, Najjar T, Boussene H, Jaafoura H, Bouguerra A, et al. Treatment of alpha chain disease. Results of a prospective study in 21 Tunisian patients by the Tunisian- French intestinal Lymphoma Study Group. Cancer. 1989;63:1251–6.
- Akbulut H, Soykan I, Yakaryilmaz F, Icii F, Aksoy F, Haznedaroglu S, et al. Five-year results of the treatment of 23 patients with immunoproliferative small intestinal disease: a Turkish experience. Cancer. 1997;80:8–14.
|