venlafaxin und alkoholvenlafaxin nedtrapning link venlafaxin depotkapsler
Institutes of Digestive and Hepatobiliary sciences,1Histopathology2
and Endocrinology3
Medanta, The Medicity, Gurgaon, Haryana, India
Corresponding Author:
Dr. NeerajSaraf
Email: neerajsaraf@hotmail.com
48uep6bbphidvals|686 48uep6bbph|2000F98CTab_Articles|Fulltext We present an interesting case of alcoholic cirrhosis with bilateral adrenal enlargement, presenting with pyrexia of unknown origin and adrenal insufficiency. Endoscopic ultrasound (EUS) has evolved as a safe and accurate modality for left adrenal FNAC. An EUS guided FNAC of the left adrenal was done, which was suggestive of adrenal histoplasmosis. The patient’s hospital course was complicated by coexisting cirrhosis. We briefly discuss adrenal histoplasmosis and advantages of EUS guided adrenal FNAC over an ultrasound or CT guided approach.
Case report
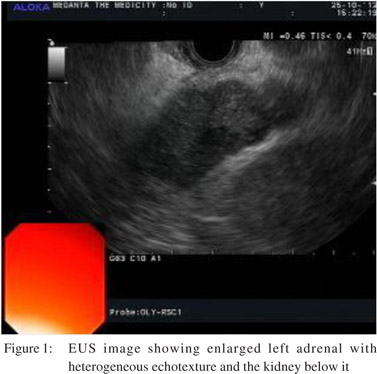
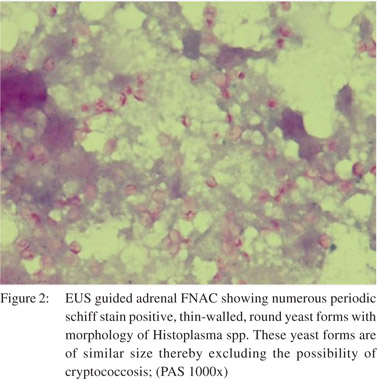
A 35-year-old patient with compensated alcoholic cirrhosis presented with fever for one month. His blood and urine cultures, widal, and peripheral smear for malaria were negative.Chest X-ray and serum iron profile were normal. On admission, his blood pressure was 90/60 mmHg, and biochemistry revealed hyponatremia (120 mEq/L), hyperkalemia (5.5 mEq/L), serum bilirubin 2.0 mg/dl, serum albumin 3.0gm/dl, INR 1.3, and serum cortisol 4.9 µg/dl. A contrast-enhanced abdominal and chest CT showed features of cirrhosis and bilateral adrenal enlargement. EUS showed 3×2.2 cm sized left adrenal with heteroechoic appearance and a maintained outline (Figure 1). EUS guided FNAC revealed numerous thin-walled round yeast forms against a necrotic background. These yeast forms were positive for periodic schiff stain and Gomori’smethanaminesilver stain with a morphology consistent with Histoplasma spp. (Figure 2). A diagnosis of adrenal insufficiency secondary to histoplasmosis was made and treatment with corticosteroids for adrenal insufficiency and liposomal amphotericin B followed by oral itraconazole for histoplasmosis was initiated. The patient’s hospital course was complicated by presence of cirrhosis.He developed high gradient ascites, hypoalbuminemia (1.8 gm/dl) and hypotension during hospital stay which improved gradually. Follow-up at 7 months showed his ascites and serum albumin levels (3.6 gm/ dl) had improved but the adrenal insufficiency persisted and he is on maintenance steroids.
Discussion
Differential diagnosis of bilateral enlarged adrenals includes neoplastic masses (malignant- metastases, adrenal carcinoma, pheochromocytoma, lymphoma, benign neoplasms like adenoma, congenital adrenal hyperplasia, macronodular adrenal hyperplasia), infections like tuberculosis, histoplasmosis, cryptococcosis, blastomycosis, penicillosis, parasitic cysts, trauma, adrenal hemorrhage, and autoimmune disease (Addison’s disease).[1,2] Tissue diagnosis can be undertaken by ultrasound, CT or endosonography (EUS) guided FNAC of adrenal glands. Various approaches have been used for ultrasound and CT guided adrenal sampling including anterior and posterior approach, transhepatic and transpancreatic route. Complications occur in 2.8 to 8.4% of cases and include pneumothorax, pain, perinephric hemorrhage, adrenal hematoma, needle-tract metastasis and pancreatitis. Complications are more common with thick needles and via thetranshepatic route.[3] EUS guided adrenal FNAC has emerged as a safe alternative to ultrasound and CT guided adrenal FNAC.[4] Left adrenal is identified at the level of celiac trunk as a ‘‘seagull’’ shaped structure with the kidney beneath it, with clockwise torque of the echoendoscope. The right adrenal is difficult to negotiate for FNAC as it is deeper and nearer to the inferior vena cava.
Advantages of the EUS guided approach include proximity to the left adrenal as only the posterior stomach wall is traversed during FNAC thus avoiding passage through other organs; real time monitoring of needle passage; it can be completed in the same session with staging; and it is highly accurate for adrenal identification (combined accuracy of three studies being 97%). In contrast, accuracy of ultrasound for adrenal identification is 70% for the left adrenal and 90% for right.[5] Hence, complication ratesare much lower with EUS FNAC than percutaneous approaches.[5]
References
- Gupta P, Bhalla A, Sharma R. Bilateral adrenal lesions. J Med Imaging Radiat Oncol. 2012;56:636–45.
- Larbcharoensub N, Boonsakan P, Aroonroch R, Rochanawutanon M, Nitiyanant P, Phongkitkarun S, et al. Adrenal histoplasmosis: a case series and review of the literature. Southeast Asian J Trop Med Public Health. 2011;42:920–5.
- Welch TJ, Sheedy PF, 2nd, Stephens DH, Johnson CM, Swensen SJ. Percutaneous adrenal biopsy: review of a 10-year experience. Radiology. 1994;193:341–4.
- Eloubeidi MA, Seewald S, Tamhane A, Brand B, Chen VK, Yasuda I, et al. EUS-guided FNA of the left adrenal gland in patients with thoracic or GI malignancies. Gastrointest Endosc. 2004;59:627–33.
- Bodtger U, Vilmann P, Clementsen P, Galvis E, Bach K, Skov BG. Clinical impact of endoscopic ultrasound-fine needle aspiration of left adrenal masses in established or suspected lung cancer. J Thorac Oncol. 2009;4:1485–9.
- Schuurbiers OC, Tournoy KG, Schoppers HJ, Dijkman BG, Timmers HJ, de Geus-Oei LF, et al. EUS-FNA for the detection of left adrenal metastasis in patients with lung cancer. Lung Cancer. 2011;73:310–5.
|