SK Mathur, Monika Sangwan, Ragini Singh, Narender Dahiya
Department of Pathology, PGIMS,
Rohtak - 124001, Haryana, India
Corresponding Author:
Dr Monika Sangwan
Email: dr.monika1311@yahoo.in
48uep6bbphidvals|675 48uep6bbph|2000F98CTab_Articles|Fulltext Splenic cysts are uncommon entities with an incidence of 0.5-2.0%.[1]Acomprehensive differential diagnosis of cystic lesions of the spleen includes parasitic echinococcal cyst, congenital cyst, intersplenic pancreatic pseudocyst, pseudocystarising from splenic trauma,necrotising infection, pyogenic splenic abscess, metastatic diseases and cystic lymphangioma or hemangioma.[2]
Case report
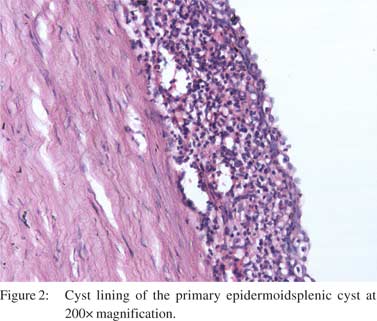
A 35-year-old male presented with complaints of abdominal discomfort and pain left hypochondriumradiating to ipsilateralshoulder. There was no history of trauma and weight loss. Physical examination revealed a large palpable ,nonmobile, firm to hardswellingin the left hypochondrium. Routine investigations were normal. An ultrasonogram (USG) revealeda well defined cystic mass.On CT scan a 14 × 12 cm cyst was localized to the spleen which had displaced the splenic parenchyma andthe possibility of a hydatid cyst was entertained. Exploratory laparotomy with splenectomy was performed. Peroperatively a large cyst sized 14 × 12cm was seen. The splenectomyspecimen was received in our pathology department,weighing 550gm and measuring 15 × 13 × 4cm. Grossly, awell encapsulated cystic area along with normal splenic tissue was identified. On cut section, the cyst had a thick wall and contained brown colored fluid. The interior surface was trabeculated (Figure 1). Microscopic examination revealed a thick fibrous wall lined by squamous epithelium (Figure 2). Focal areas of calcification were also present. Immunohistochemistry was positive for cytokeratin (CK) (Figure 3) and negative for calretinin. The final diagnosis of a primary epidermoid cyst of spleen was made.

 Discussion
Fowler in 1953 reviewed 265 cases from global literature and proposed the first pathological classification for splenic cysts, dividing them into parasitic (75%) and non-parasitic cysts (25%)[3]. Non-parasitic cysts are further classified as primary or secondary cysts. Secondary cysts are associated with splenic trauma or hemorrhage. No epithelial lining is present in these and the cyst wall is composed of dense fibrous tissue with 25% of cases showing areas of calcification. A primary or true cyst on the other hand has a thick fibrous wallwhich is at least partially surfaced by amesothelialand/or a squamous epithelial layer.[4]Depending on the type of lining they are classified as epidermoid, dermoid and mesothelial cysts.[5]
Discussion
Fowler in 1953 reviewed 265 cases from global literature and proposed the first pathological classification for splenic cysts, dividing them into parasitic (75%) and non-parasitic cysts (25%)[3]. Non-parasitic cysts are further classified as primary or secondary cysts. Secondary cysts are associated with splenic trauma or hemorrhage. No epithelial lining is present in these and the cyst wall is composed of dense fibrous tissue with 25% of cases showing areas of calcification. A primary or true cyst on the other hand has a thick fibrous wallwhich is at least partially surfaced by amesothelialand/or a squamous epithelial layer.[4]Depending on the type of lining they are classified as epidermoid, dermoid and mesothelial cysts.[5]
Epidermoidcyst of spleen is a rare primary cyst. These are common in thesecond and third decades of life, but can occur at any age. Male predominance has been suggested. An abdominal mass is the most common presentation accompaniedby abdominalpain or gastrointestinal disturbances.[6] Onultrasonography, epidermoid cysts appear as well defined thin walled anechoic lesions. On CT scan, they manifest as rounded, well demarcated non-enhancing water attenuation lesions. Sonographic and CT scan findings are not specificand various cysts may present with similar appearance.Complications of cysts include rupture, infection and intracystic hemorrhage. Spontaneous rupture of a splenic cyst can cause massive haemoperitoneum or peritonitis. If the cyst is small (<5cm) no treatment is needed. If it is bigger than 5cm, is located at the hilum or is causing complicationsthen surgery is the gold standard line of management. Differen modalities include splenectomy, partialsplenectomy, cystectomy, partial cystectomy or splenic decapsulation.[4] Microscopicallythe presence of an epithelial lining confirms the cyst as a primary splenic cyst. The final diagnosis can only be made at histopathology and confirmed by immunohistochemistry.
References
- Higaki K, Jimi A, Watanabe J, Kusaba A, Kojiro M. Epidermoid cyst of the spleen with CA19-9 or carcinoembryonic antigen productions: report of three cases. Am J SurgPathol. 1998;22:704–8.
- Daga G, Mittal V, Singh RJ, Sood N. Epithelial cyst of the spleen. J Indian AssocPediatr Surg. 2011;16:18–20.
- Fowler RH. Nonparasitic benign cystic tumors of the spleen. Int Abstr Surg. 1953;96:209–27.
- Macheras A, Misiakos EP, Liakakos T, Mpistarakis D, Fotiadis C, Karatzas G. Non-parasitic splenic cysts: a report of three cases. World J Gastroenterol. 2005;11:6884–7.
- Palmieri I, Natale E, Crafa F, Cavallaro A, Mingazzini PL. Epithelial splenic cysts. Anticancer Res. 2005;25:515–21.
- El-Khoury EF, Souaiby MC, Aftimos GP. Epidermoid cyst of the spleen: case report. J Med Liban. 2009;57:268–70.
|