Sushma Patra1,4 Mukul Vij1, Dharmesh Kapoor2, Mohamed Rela3
Departments of Pathology,1 and
Liver Transplantation and
Hepatobiliary Surgery,3
Global Hospital and Health City,
Chennai, Tamilnadu - 600100, India
Department of Hepatology,2 Global Hospital,
Hyderabad, Andhra Pradesh, India
Department of Pathology,4
AIIMS, Bhubaneswar,
Odisha - 751019, India
Corresponding Author:
Dr. Sushma Patra
Email: wususama@gmail.com
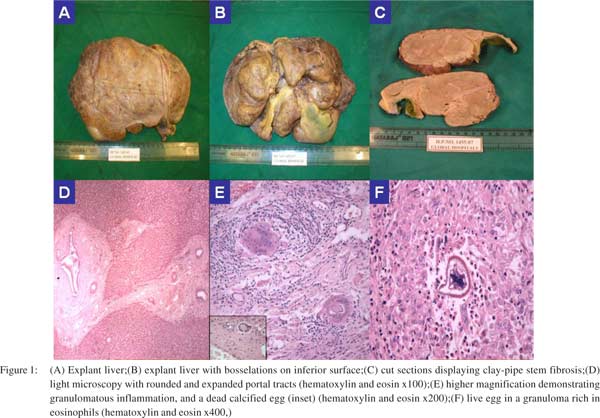
48uep6bbphidvals|670 48uep6bbph|2000F98CTab_Articles|Fulltext A 48-year-old man from the Middle-East presented to us with a history of severe portal hypertension, leading to refractory GI bleed not responding to therapy. On examination there was massive splenomegaly with minimal ascites. Magnetic resonance imaging revealed minimally shrunken liver with nodular regenerative hyperplasia. All autoimmune and viral markers were negative. Serum alpha-feto protein and CA 19-9 were within normal limits. Orthotopic live related liver transplant was done. We received a firm enlarged liver weighing 1175 grams and measuring 27×17×6cm. The liver showed a thickened capsule and bosselations on its inferior surface (Figure 1A, 1B). On cut section, there were round to stellate shaped,thick, grayish-white tracts of collagen around major portal tracts, which is described as Symmers’ clay-pipe stem fibrosis (Figure 1C). The liver architecture was preserved and there was no cirrhosis. Histology revealed portal expansion with fibrosis. Within the fibrous septa tortuous arterioles and venules, entrapped bile ductules, along with granulomatous eosinophil-rich inflammation and dead calcified eggs were noted (Figure 1D, 1E). Occasional granuloma containing live eggs with shell and spine and the circular ring of nuclei were also identified (Figure 1F).Schistosomal haemozoin pigment phagocytosed by macrophages was visible within the portal tracts and sinusoidal Kupffer cells. Few portals tracts also showed evidence of venosclerosis with loss of venules with or without proliferation of abnormal vessels with focal cavernous transformation. We labeled the explant liver with hepatic schistosomiasis. Schistosomiasis or bilharzia is a tropical parasitic disease caused by blood-dwelling flukes of the genus Schistosoma. S. mansoni, S. japonicum, S. mekongi and S. intercalatum infections are associated with chronic hepaticfibrosis.[1] The main pathogenic lesions in chronic infection are not due to the adult worms but because of eggs that are trapped in tissues due to peri-intestinal migration or embolization to liver, spleen, lungs, or the cerebrospinal system. The eggs secrete proteolytic enzymes that provoke typical eosinophilic inflammatory and granulomatous reactions, which are progressively replaced by fibrosis.
 References
References
- Gryseels B, Polman K, Clerinx J, Kestens L. Human schistosomiasis. Lancet. 2006;368:1106–18.
|