Abhay Kumar Kapoor1, Ankur Arora2, Ashok Sharma1
Department of Radiodiagnosis,
G.B Pant Hospital,1
Department of Radiodiagnosis,
Institute of Liver and Biliary Sciences,2
New Delhi, India
Corresponding Author:
Dr. Abhay Kumar Kapoor
Email: drabhaykapoor@gmail.com
48uep6bbphidvals|667 48uep6bbph|2000F98CTab_Articles|Fulltext Hepatic hemangiomas are the most common benign hepatic masses with a prevalence of 1-20%.[1] They are more commonly seen in females than males with a ratio varying from 2:1 to 5:1.[1] Typical radiographic characteristics of hepatic hemangiomas are well described and extremely specific. However, intratumoral structural variation may cause unusual imaging features. This can lead to misleading diagnosis. Hence, knowledge of imaging features of atypical hemangiomas is imperative to avoid unnecessary interventions.
Case report
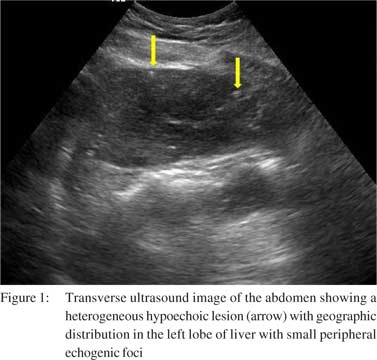
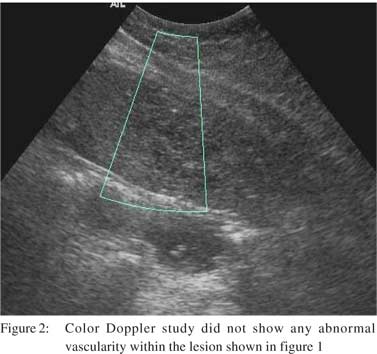
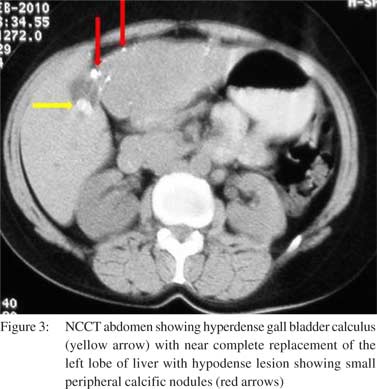
A 46year-old female patient presented with history of pain in right hypochondrium since four months. The pain was associated with two episodes of vomiting over last three days. There was no history of fever. On examination, mild hepatomegaly was noted with tenderness in right hypochondrium. Liver function tests were normal. Ultrasound abdomen revealed a large calculus impacted in the gall bladder neck. However, there was no evidence of any wall thickening or pericholecystic collection. The liver showed a heterogeneous hypoechoic lesion with geographic distribution in the left lobe with few similar smaller areas in the right lobe also. Small peripheral echogenic foci were noted which did not cast a distal acoustic shadow (Figure 1). These lesions did not show any abnormal vascularity on color Doppler scan, neither within the lesion nor at their periphery (Figure 2). In view of the heterogeneous multifocal lesions in the liver, a CT scan was advised. The plain scan revealed near complete replacement of the left lobe of liver with a hypodense lesion showing small peripheral calcific nodules along with few similar low density round lesions in the right lobe (Figure 3).
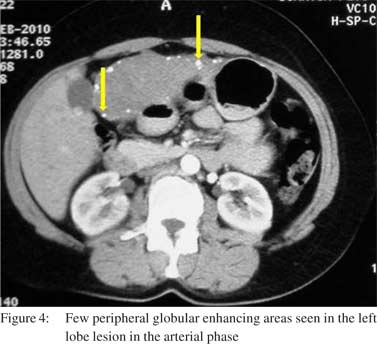
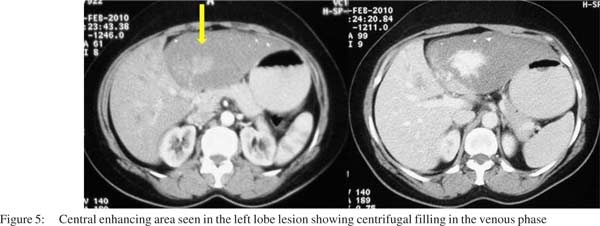
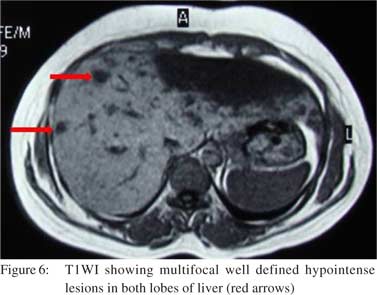
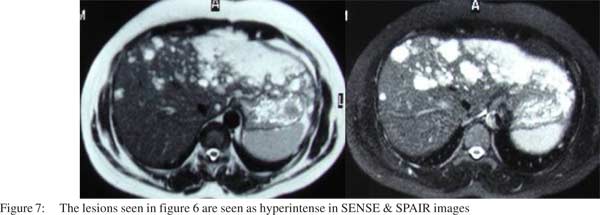
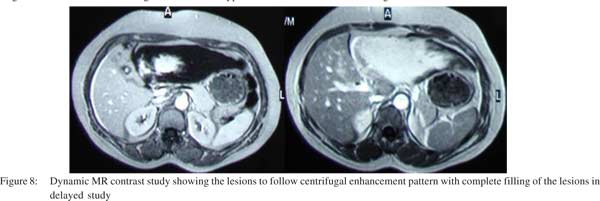
 Few peripheral globular enhancing areas were seen in the left lobe lesion in the arterial phase along with the central enhancing area (Figure 4). Few right lobe lesions also showed central enhancing nodular areas. The venous phase showed centrifugal enhancement in all the lesions (Figure 5). A diagnosis of atypical hemangioma was considered at this stage and an MRI was done. The MRI showed the lesions to be hypointense on T1WI (Figure 6) and as hyperintense as CSF on T2WI (Figure 7). Dynamic MR contrast study showed the lesions to follow a centrifugal enhancement pattern with complete filling of the lesions in delayed study (Figure 8). An FNAC from the lesion confirmed the diagnosis of hemangioma.
Few peripheral globular enhancing areas were seen in the left lobe lesion in the arterial phase along with the central enhancing area (Figure 4). Few right lobe lesions also showed central enhancing nodular areas. The venous phase showed centrifugal enhancement in all the lesions (Figure 5). A diagnosis of atypical hemangioma was considered at this stage and an MRI was done. The MRI showed the lesions to be hypointense on T1WI (Figure 6) and as hyperintense as CSF on T2WI (Figure 7). Dynamic MR contrast study showed the lesions to follow a centrifugal enhancement pattern with complete filling of the lesions in delayed study (Figure 8). An FNAC from the lesion confirmed the diagnosis of hemangioma.
Discussion
Hepatic hemangiomas can have varied imaging appearances making it difficult at times to differentiate them from malignant masses. Imaging is fairly accurate in diagnosing typical hemangiomas with MRI being the modality of choice with a sensitivity and specificity above 90%.[1]
The varied imaging appearances are due to different structural composition of the lesions. Hemangiomas showing rapid enhancement have relatively large vascular spaces with thin intervening septae whereas hemangiomas with slow filling pattern have small vascular spaces with a large portion of
fibrous interstitial spaces.[2] The signal intensity characteristics on MRI are related to relative composition of intralesional vascular spaces, connective tissue, presence of thrombosis, calcification, hemorrhage, or fibrosis. Imaging characteristics of hemangioma have shown correlation with their size, with typical features seen in most lesions less than 3 cm in diameter.[3] The typical hemangioma appears as an echogenic lesion on USG showing posterior acoustic enhancement. On CT scan it appears as a hypodense lesion showing peripheral globular enhancement in arterial phase with gradual complete filling in centripetal manner in delayed images. On MRI the typical hemangioma appears hypointense on T1WI and hyperintense as CSF on T2WI. The light bulb sign on T2WI has been linked to benign hepatic lesion like cysts or hemangioma. However, its absence is more specific for malignant lesion as this sign may be seen in some malignant lesions also.[4]
Atypical hepatic hemangiomas may present with an echogenic border and central hypoechoic area on USG. This appearance is noted in up to 40% of cases.[5] Hemangiomas may be large and heterogeneous when they are called giant hemangiomas. The criteria to call the lesion as giant hemangioma varies in different text. Its size should be more than 4 cm, 6 cm or 12 cm.1 We may have rapidly filling hemangiomas. This pattern is seen more commonly in lesions smaller than 1 cm. It is seen in up to 16% of cases. These need to be differentiated from hypervascular malignancies. In a retrospective study done by Outwater et al,[6] it was seen that T2-weighted images and dynamic gadolinium-enhanced images could very accurately distinguish the two lesions with high accuracy (97-100%) as signal intensity on the heavily T2- weighted images of the hemangiomas was significantly greater than that of hypervascular malignant lesions (p <0.05). Although hemangiomas may not show any enhancement but once they enhance they do not show washout as seen in malignant lesions.[7]
There has been one case report of hemangioma presenting with peripheral rim enhancement on dynamic CT scan mimicking hepatocellular carcinoma.[8] This may be attributed to the surrounding liver parenchymal fibrotic change caused by an active hepatitis C viral infection. There may be calcified hemangioma, hyalinized hemangioma, cystic or multilocular hemangioma. Only one case of multilocular hemangioma is reported.[1] Calcification may be seen in the lesion’s periphery in a spotty nodular form representing phleboliths or they may be large and organized. Hyalinised hemangiomas are not as hyperintense as the typical hemangioma on T2WI. These do not show early enhancement in dynamic contrast study and can be difficult to differentiate from malignant lesions. Hemangiomas may present with a fluid-fluid level. Two such cases have been reported.[1] This is most likely due to bleed within the hemangioma forming a lower layer of stagnant blood and upper layer of serous unclotted blood. Pedunculated appearance of hemangioma is also known where the thin pedicle with the liver may not be discernible on imaging and the diagnosis is made on the basis of the typical enhancement pattern. Arterial–portal venous shunting is also seen in hemangiomas with a total of fourteen cases reported with this appearance.[1] Hemangiomas may present with capsular retraction and confuse with cholangiocarcinoma.
Lastly, hemangiomas may present with atypical inside-out pattern showing centrifugal enhancement pattern on dynamic contrast-enhanced CT and MR imaging. Two such cases have been reported in CT/MR imaging by Kim et al,[2] one by Hosokawa et al,[9] and one on CT scan by Matsushita et al.[10] Bartolotta et al reported a series of seven patients with this atypical pattern on contrast USG.[11] The lesion reported by Hosokawa et al was exophytic and showed centrifugal enhancement along with dilatation of the right posterior inferior branch of the hepatic artery on angiography. Matsushita et al performed dynamic computed tomography during hepatic arteriography and demonstrated a centrifugal enhancement pattern with subsequent peri-tumoral ring-shaped enhancement mimicking corona enhancement in a cavernous hemangioma of a 68-yearold man. Bartolotta et all conducted contrast enhanced USG in 92 cases of atypical appearing hemangiomas on USG and found 12 out of 158 lesions to show central enhancing focus in arterial phase followed by centrifugal enhancement in the portal venous and delayed phases.[11]
References
- Vilgrain V, Boulos L, Vullierme MP, Denys A, Terris B, Menu Y. Imaging of atypical hemangiomas of the liver with pathologic correlation. Radiographics. 2000;20:379–97.
- Kim S, Chung JJ, Kim MJ, Park S, Lee JT, Yoo HS. Atypical inside-out pattern of hepatic hemangiomas. AJR Am J Roentgenol. 2000;174:1571–4.
- Nelson RC, Chezmar JL. Diagnostic approach to hepatic hemangiomas. Radiology. 1990;176:11–3.
- Wittenberg J, Stark DD, Forman BH, Hahn PF, Saini S, Weissleder R, et al. Differentiation of hepatic metastases from hepatic hemangiomas and cysts by using MR imaging. AJR Am J Roentgenol. 1988;151:79–84.
- Moody AR, Wilson SR. Atypical hepatic hemangioma: asuggestive sonographic morphology. Radiology. 1993;188:413–7.
- Outwater EK, Ito K, Siegelman E, Martin CE, Bhatia M, Mitchell DG. Rapidly enhancing hepatic hemangiomas at MRI: distinction from malignancies with T2-weighted images. J Magn Reson Imaging. 1997;7:1033–9.
- Jang HJ, Kim TK, Lim HK, Park SJ, Sim JS, Kim HY, et al. Hepatic hemangioma: atypical appearances on CT, MR imaging, and sonography. AJR Am J Roentgenol. 2003;180:135–41.
- Tsurusaki M, Kawasaki R, Yamaguchi M, Sugimoto K, Fukumoto T, Ku Y, et al. Atypical hemangioma mimicking hepatocellular carcinoma with a special note on radiological and pathological findings. Jpn J Radiol. 2009;27:156–60.
- Hosokawa A, Maeda T, Tateishi U, Satake M, Iwata R, Ojima H, et al. Hepatic hemangioma presenting atypical radiologic findings: a case report. Radiat Med. 2005;23:371–5.
- Matsushita M, Takehara Y, Nasu H, Hirai Y, Yamashita S, Souda K, et al. Atypically enhanced cavernous hemangiomas of the liver: centrifugal enhancement does not preclude the diagnosis of hepatic hemangioma. J Gastroenterol. 2006;41:1227–30.
- Bartolotta TV, Taibbi A, Galia M, Lo Re G, La Grutta L, Grassi R, et al. Centrifugal (inside-out) enhancement of liver hemangiomas: a possible atypical appearance on contrastenhanced US. Eur J Radiol. 2007;64:447–55.
|