Nihar Ranjan Dash1, Nikhil Agrawal1, Manik Sharma2, Amit Javed1
Departments of Gastrointestinal Surgery1 and Gastroenterology,2
All India Institute of Medical Sciences,
Ansari Nagar, New Delhi - 110029, India
Corresponding Author:
Dr. Nihar Ranjan Dash
Email: nagranjan@gmail.com
48uep6bbphidvals|634 48uep6bbph|2000F98CTab_Articles|Fulltext Impaction of a wide range of foreign bodies in the oesophagus has been described in the literature. These are retrieved either by endoscopy or surgery. We report impaction of an unusual foreign body (mango seed) in the oesophagus which could not be extracted endoscopically. A thoracotomy/oesophagotomy would have been too morbid for the elderly patient. A rendezvous approach using endoscopy and surgery successfully retrieved the foreign body avoiding a thoracotomy.
Case report
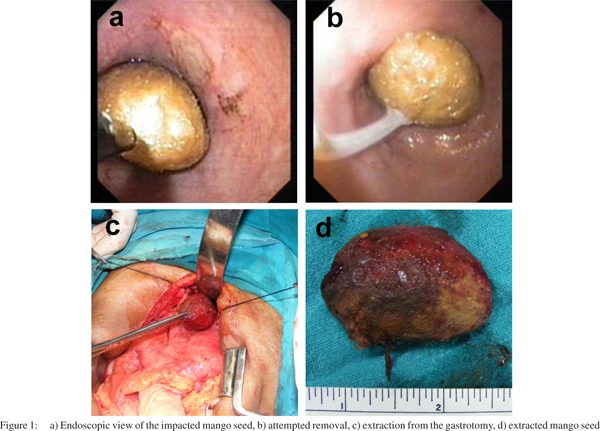
An 80-year-old man presented to the All India Institute of Medical Sciences, New Delhi with a 10 day history of dysphagia and chest pain. He was able to swallow liquids with difficulty. On further questioning he gave history of accidental ingestion of a mango seed 10 days ago. There were no other complaints. His physical examination was unremarkable. Chest and abdominal X-rays were normal. An upper gastrointestinal endoscopy revealed a large mango seed impacted at 30 cm from the incisors (Figure 1a) but it could not be extracted (Figure 1b). An attempt to retrieve it using a snare and a gentle push also failed. Forceful dislodgement was not attempted given the long duration of impaction, the size of foreign body and the possibility of a distal lesion. A surgical extraction was planned but as the patient was elderly, it was decided to avoid a thoracotomy and oesophagotomy. At laparotomy, the seed could not be felt at the gastroesophageal junction. A gastrotomy was made in the upper body of the stomach and after placing retractors within the stomach, the tip of the seed was just visible.
Endoscopy from below showed no evidence of any narrowing or growth in the distal oesophagus. An attempt to grasp the seed was unsuccessful. An upper gastrointestinal endoscope was passed through the oesophagus and the seed was pushed with the endoscope. This manoeuvre succeeded in prolapsing a part of the seed along with the oesophageal mucosa into the gastroesophageal junction allowing the seed to be grasped at its widest part with a long Allis forceps. The seed was then gently dislodged with a to-and-fro motion and extracted from the gastrotomy (Figure 1c-d). The oesophagus at the site of impaction was normal but a mucosal biopsy was obtained. Full oral diet was established by fourth postoperative day. He was discharged on the seventh postoperative day without any complications. The biopsy did not show any evidence of malignancy.
 Discussion
The oesophagus is the most common site of lodgement of foreign bodies in the gastrointestinal tract accounting for approximately 75% of all impactions.[1] Most foreign bodies pass spontaneously, with only 10-20% requiring some form of intervention.[2] Foreign body impactions in the oesophagus are more common in children. In adults they are seen more often in edentulous and elderly people with an impaired mental status, prison inmates, patients with narrowing of the oesophagus and those with oesophageal motility disorders. Acute onset dysphagia or inability to swallow saliva is the key symptom. Our patient presented when he developed significant dysphagia, 10 days after ingestion of the mango seed.
Discussion
The oesophagus is the most common site of lodgement of foreign bodies in the gastrointestinal tract accounting for approximately 75% of all impactions.[1] Most foreign bodies pass spontaneously, with only 10-20% requiring some form of intervention.[2] Foreign body impactions in the oesophagus are more common in children. In adults they are seen more often in edentulous and elderly people with an impaired mental status, prison inmates, patients with narrowing of the oesophagus and those with oesophageal motility disorders. Acute onset dysphagia or inability to swallow saliva is the key symptom. Our patient presented when he developed significant dysphagia, 10 days after ingestion of the mango seed.
Oesophageal foreign bodies may be food bolus impaction (seen in patients with pathological narrowing or a motility disorder) or foreign bodies. In a series from China underlying conditions included oesophageal carcinoma (33%), stricture (23.9%), diverticulum (15.9%), postgastrectomy (11.4%), hiatus hernia (10.2%) and achalasia (5.7%).[3] Complications of foreign body impaction include ulcer formation, lacerations, perforation, intestinal obstruction, aortoesophageal fistula, tracheoesophageal fistula and bacteremia. The patient described in this report had an unusual foreign body. Till date, only one case describing impaction of a mango seed has been reported.[4] Like other vegetable foreign bodies a mango seed swells up by absorbing water compounding the impaction. The hard and even surface along with its typical configuration makes it difficult to extract unless it can be grasped at the centrally thickened portion. We did not do a CT scan in this patient because (i) he had no history suggestive of prior oesophageal disease or any complication of impaction such as perforation, (ii) he merited retrieval and (iii) intraoperative endoscopic retrieval/assessment was planned.
Under no circumstances should a foreign body be allowed to remain in the oesophagus beyond 24 hours from presentation.[5] Endoscopic retrieval using a forward viewing flexible endoscope is the preferred modality of treatment in most cases and a success rate of 98% has been reported.[1,6] Push technique has also been described wherein the foreign body may be pushed into the stomach.[7]This should however be attempted only when the foreign body is not sharp, is expected to spontaneously pass down the distal gastrointestinal tract (<2.5 cm), and in the absence of oesophageal obstruction distal to the site of impaction. All endoscopic manoeuvres to extract the seed failed in our patient due to its large size and inability to achieve a good grasp on it. Surgical intervention is indicated when endoscopic techniques fail or if there are complications like obstruction, perforation or gastrointestinal bleeding. There is scarcity of contemporary data on surgical management of oesophageal foreign bodies. In a series of 815 patients with oesophageal foreign bodies, four (0.5%) required oesophagotomy (one cervical and three thoracic). One suture line dehiscence occurred. The authors postulated that occult foreign body pressure necrosis may be a factor in oesophagotomy suture line leakage.[8] In another series of 400 oesophageal foreign bodies, 12 (3%) required surgery. A cervical oesophagotomy, left thoracotomy, right thoracotomy and a gastrotomy was required in six, four, one and one cases, respectively. No major complication was reported.[9]
Most patients require a thoracotomy and an oesophagotomy but is associated with significant morbidity especially in the elderly. In our patient, we were able to avoid this procedure. An upper midline laparotomy, a high gastrotomy and a combined rendezvous approach resulted in smooth retrieval of the impacted mango seed and avoided the morbidity of a thoracotomy and oesophagotomy in an 80-year-old patient.
References
- Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995;41:39–51.
- Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc. 1995;41:33–8.
- Li ZS, Sun ZX, Zou DW, Xu GM, Wu RP, Liao Z. Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in China. Gastrointest Endosc. 2006;64:485–92.
- Misra SP, Dwivedi M. Removal of a mango seed from the esophagus using a specially designed retrieval device. Endoscopy. 1996;28:399.
- Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002;55:802–6.
- Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: epidemiology and therapy. A retrospective, observational study. Gastrointest Endosc. 2001;53:193–8.
- Vicari JJ, Johanson JF, Frakes JT. Outcomes of acute esophageal food impaction: success of the push technique. Gastrointest Endosc. 2001;53:178–81.
- Stewart KC, Urschel JD, Fischer JD, Geeraert AJ, Lees GM, Mossey JF. Esophagotomy for incarcerated esophageal foreign bodies. Am Surg. 1995;61:252–3.
- Athanassiadi K, Gerazounis M, Metaxas E, Kalantzi N. Management of esophageal foreign bodies: a retrospective review of 400 cases. Eur J Cardiothorac Surg. 2002;21:653–6.
|