Madhukar Dayal1, Raju Sharma1, Nadarajah Jeyaseelan1, Rita Sood2, Sandeep R. Mathur3,Sanjeev Chitragar3
Department of Radiodiagnosis1,
Medicine2, and Pathology3,
AIIMS, New Delhi - 110029, India
Corresponding Author:
Dr Raju Sharma
Email: raju152@yahoo.com
48uep6bbphidvals|618 48uep6bbph|2000F98CTab_Articles|Fulltext Blunt abdominal trauma is the most common cause of splenic rupture. Non-traumatic splenic rupture is rare and occurs in a diseased spleen. Among the non-traumatic causes, haematological malignancy is the leading cause of splenic rupture; others being infection, malignancy, vascular, genetic or haematological disorders.[1] However, in countries where malaria is endemic, it outnumbers haematological malignancy as the leading cause of splenic rupture.[1,2] We report a case of non-traumatic rupture of the spleen with a large subcapsular splenic haematoma and haemoperitoneum in a patient suffering from acute malaria.
Case report
A 27-year-old man presented to the emergency department with pain in the left hypochondrium and distention of the abdomen. The patient gave a history of intermittent high-grade fever with chills and rigor for the past 4 days. There was no history of any trauma or abnormal bleeding tendency. The patient was receiving antimalarial treatment for diagnosed Plasmodium vivax infection (seen on peripheral blood smear), which was prescribed to him by a local physician. On clinical examination, the patient had pallor and tachycardia with a normal blood pressure and local tenderness in the left hypochondrium, but there was no abdominal guarding or rigidity. Blood/serum profile showed dimorphic anaemia with increased serum bilirubin level (2.7 mg/dL) and low platelet count (90,000/dL). The Widal test was negative.
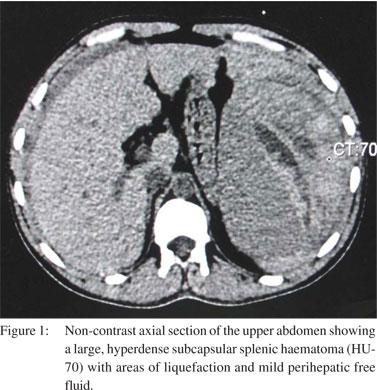
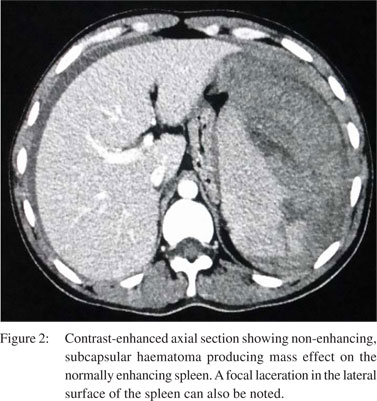
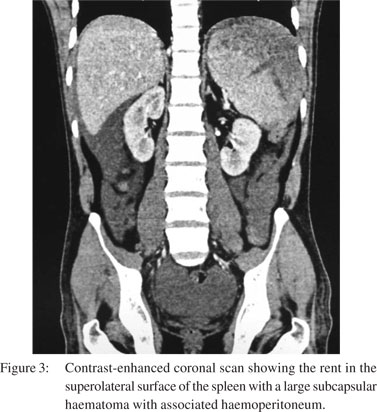
Ultrasonography (USG) revealed a large, subcapsular splenic haematoma with free fluid in the abdomen consistent with haemoperitoneum. Computed tomography (CT) scan confirmed the presence of a large, subcapsular splenic haematoma (hyperdense on non-contrast CT scan, 70 Hounsfield units) with extension into the perisplenic and left subdiaphragmatic region) with free fluid in the abdomen (Figures 1–3). The patient underwent an urgent splenectomy and the histopathology report revealed the presence of malarial pigment in the ruptured spleen (Figure 4).
 Discussion
Malaria is a parasitic infection caused by Plasmodium species. In India, P. vivax accounts for approximately 55% of cases whereas 40%–42% of cases are caused by P. falciparum which is most frequently associated with severe complicated malaria.[1] Infections by other two species are often subclinical and associated with fewer complications. However, splenic complications are commonly associated with non-falciparum species especially P. vivax. They occur in up to 2% of cases.[3,4] Patients may present with left hypochondriac pain which may be due to infarct in an enlarged spleen, trauma to an enlarged spleen and rarely rupture of the spleen. Most cases of splenic rupture occur during acute infection. Although there is considerable splenomegaly in chronic malaria, rupture is uncommon as excessive fibrosis acts as a protective barrier against rupture. In cases with acute disease, there is rapid enlargement and stretching of splenic capsule secondary to vascular congestion and cellular hyperplasia, and the lack of fibrosis predisposes to splenic rupture. Diagnosis should always be suspected in a patient from an endemic region who presents with rapid onset of hypotension and severe left hypochondrial pain. Abdominal USG is a rapid bedside modality for assessing the severity of splenic rupture, amount of subcapsular and intraperitoneal haematoma. It also helps to exclude other causes which may present with left hypochondrial pain such as left-sided pleural pathology, pancreatitis and renal calculi. In haemodynamically stable patients, CT scan can be performed to delineate the findings and a better assessment of their severity.[2–5]
References
Discussion
Malaria is a parasitic infection caused by Plasmodium species. In India, P. vivax accounts for approximately 55% of cases whereas 40%–42% of cases are caused by P. falciparum which is most frequently associated with severe complicated malaria.[1] Infections by other two species are often subclinical and associated with fewer complications. However, splenic complications are commonly associated with non-falciparum species especially P. vivax. They occur in up to 2% of cases.[3,4] Patients may present with left hypochondriac pain which may be due to infarct in an enlarged spleen, trauma to an enlarged spleen and rarely rupture of the spleen. Most cases of splenic rupture occur during acute infection. Although there is considerable splenomegaly in chronic malaria, rupture is uncommon as excessive fibrosis acts as a protective barrier against rupture. In cases with acute disease, there is rapid enlargement and stretching of splenic capsule secondary to vascular congestion and cellular hyperplasia, and the lack of fibrosis predisposes to splenic rupture. Diagnosis should always be suspected in a patient from an endemic region who presents with rapid onset of hypotension and severe left hypochondrial pain. Abdominal USG is a rapid bedside modality for assessing the severity of splenic rupture, amount of subcapsular and intraperitoneal haematoma. It also helps to exclude other causes which may present with left hypochondrial pain such as left-sided pleural pathology, pancreatitis and renal calculi. In haemodynamically stable patients, CT scan can be performed to delineate the findings and a better assessment of their severity.[2–5]
References
- Gupta N, Lal P, Vindal A, Hadke NS, Khurana N. Spontaneous rupture of malarial spleen presenting as hemoperitoneum: a case report. J Vector Borne Dis. 2010;47;119–20.
- Choudhury J, Uttam KG, Mukhopadhyay M. Spontaneous rupture of malarial spleen. Indian Pediatr. 2008;45:327–8.
- Yagmur Y, Kara IH, Aldemir M, Büyükbayram H, Tacyildiz IH, Keles C. Spontaneous rupture of malarial spleen: two case reports and review of literature. Crit Care. 2000;4:309–13.
- Tauro LF, Maroli R, D’Souza CR, Hedge BR, Shetty SR, Shenoy D. Spontaneous rupture of the malarial spleen. Saudi J Gastroenterol. 2007;13:163–7.
- Correia M, Amonkar D, Audi P, Kudchadkar S. Spontaneous rupture of a malarial spleen—a case report and review of literature. Internet J Surg. 2010;23. Doi:10.5580/1aa8.
|