Suddhasatta Ghosh1, Suparna Guha1, Sumita Basu1, Dilip Kumar Mukherjee1, Riddhi Das Gupta2
Department of Paediatrics1,
Vivekananda Institute of Medical Science,
Department of Endocrinology2,
NRS Medical College, Kolkata,
West Bengal, India
Corresponding Author:
Suddhasatta Ghosh
Email: riddhi_dg@rediffmail.com
48uep6bbphidvals|617 48uep6bbph|2000F98CTab_Articles|Fulltext Case report
A 1-year-old girl child of non-consanguinous parents presented with a history of regurgitation of feeds and poor weight gain lasting for the past 6 months. Initially, she used to regurgitate unaltered solid foods immediately after ingestion. Later she started regurgitating both solid and liquid food and her condition gradually worsened. She also suffered from two bouts of pneumonia in the past 4 months. She had numerous medical consultations and got treated for gastro-oesophageal reflux but with no improvement. There was no significant birthor neonatal- or family history related to her illness.
On examination, the infant was malnourished and pale with a weight of 5.5 kg (below the 3rd percentile) and a length of 55 cm (below the 3rd percentile). Examination of other systems was unremarkable.
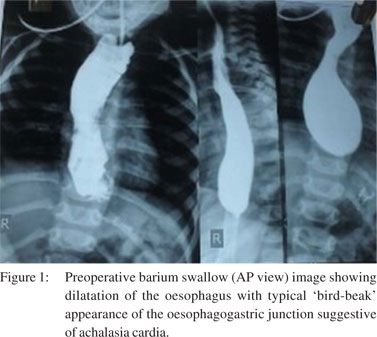
Routine blood investigations were within normal limits. We proceeded for an upper gastrointestinal (GI) endoscopy but the endoscope could not be advanced beyond the gastrooesophageal junction. Subsequently, barium swallow study was done and it revealed a dilated oesophagus and typical “bird-beak” appearance of the oesophagogastric junction with delayed passage of barium into the stomach (Figure 1). Motility study could not be done because of technical difficulty in performing oesophageal manometry in the child. Diagnosis of achalasia cardia was based on clinical grounds and barium swallow images.
As symptoms persisted, the infant underwent a modified Heller anterior oesophagocardiomyotomy through the abdominal route with short-wrap Nissen fundoplication. The nasogastric tube was removed on postoperative day 4 and the child could resume normal feeding from the following day. Barium swallow studies done after one week of the operation showed a free passage of barium into the stomach. The followup examination has revealed dramatic relief of symptoms and satisfactory weight gain.
Discussion
 Oesophageal achalasia is a relatively rare problem in children with less than 250 cases reported in the world literature till 1988.[1] A search of the English literature revealed only 30 cases of achalasia in infancy reported so far. The first case was probably reported by King in 1953.[2] A similar case of achalasia cardia in a 7-month-old infant was reported from the Christian Medical College, Ludhiana, Punjab, India by Sarin and Stephen in 1997.[3] In 2010, Sarangapani et al. reported a case of a 6- month-old male infant with achalasia from Sri Ramchandra Medical College, Chennai, India.[4] The infant underwent a modified Heller anterior oesophagocardiomyotomy with fundoplication and had excellent postoperative recovery. However, achalasia cardia in infants is a rarity. In fact, the two largest institutional series ever reported comprised only 4 patients each.[5,6] This results in delayed diagnosis in many instances.
References
Oesophageal achalasia is a relatively rare problem in children with less than 250 cases reported in the world literature till 1988.[1] A search of the English literature revealed only 30 cases of achalasia in infancy reported so far. The first case was probably reported by King in 1953.[2] A similar case of achalasia cardia in a 7-month-old infant was reported from the Christian Medical College, Ludhiana, Punjab, India by Sarin and Stephen in 1997.[3] In 2010, Sarangapani et al. reported a case of a 6- month-old male infant with achalasia from Sri Ramchandra Medical College, Chennai, India.[4] The infant underwent a modified Heller anterior oesophagocardiomyotomy with fundoplication and had excellent postoperative recovery. However, achalasia cardia in infants is a rarity. In fact, the two largest institutional series ever reported comprised only 4 patients each.[5,6] This results in delayed diagnosis in many instances.
References
- Vane DW, Cosby K, West K, Grosfeld JL. Late results following esophagomyotomy in children with achalasia. J Pediatr Surg. 1988;23:515–19.
- King R. Surgical correction of achalasia of the esophagus in infants. J Med Assoc Ga. 1953;42:466–8.
- Sarin YK, Stephen E. Achalasia cardia in an infant. Indian Pediatr. 1997;34:251–4.
- Sarangapani A, Vijayaraghavan S, Shanmuganathan S, Rajanikanth S. Achalasia cardia in an infant. Sri Lanka Journal of Child Health. 2010;40:74–5.
- Azizkhan RG, Tapper D, Eraklis A. Achalasia in childhood: a 20- year experience. J Pediatr Surg. 1980;15:452–6.
- Nihoul-Fekete C, Nihoul FC, Bawab F, Loratat-Jacob S, Arhan P, Pellerin D. Achalasia of the esophagus in childhood: surgical treatment in 35 cases with special reference to familial cases and glucocorticoid deficiency association. J Pediatr Surg. 1989;24:1060–3.
|