Introduction
Upper gastrointestinal hemorrhage is the commonest gastrointestinal emergency presenting as hematemesis, melena or both. Upper gastrointestinal bleeding (UGIB) is arbitrarily defined as bleeding from a source proximal to the ligament of Treitz.[
1] The reported incidence in the United States remains between 0.8 and 1.0 per 1000 person-years.[
2,
3] It is responsible for over 250, 000–300, 000 hospital admissions and $2.5 billion in costs in the USA each year.[
4-
6] There is very scanty data on the burden of UGIB from India. In an earlier study from coastal Odisha, UGIB accounted for 4.6% of all hospital admissions to medical wards.[
7] The spectrum of causes of UGIB varies by region and center according to healthcare hierarchy. Gastrointestinal endoscopy remains the diagnostic and therapeutic procedure of choice for UGIB. Despite advances in the diagnosis and management of UGIB, the mortality from acute UGI bleeding remains 10%–15%.[
6] The present study was carried out to determine the etiologic spectrum of UGIB in coastal Odisha and to compare it with the reported spectrum from other regions of India.
Material and Methods
The study material consisted of the clinical and endoscopic data obtained from consecutive patients with UGIB coming to the gastroenterology outpatient clinic, Digestive Diseases Centre, Cuttack in coastal Odisha over a period of 3 years (2007-2010). The data analyzed included the detailed history of GI bleeding, alcoholism and NSAID use. All patients underwent thorough physical exam, and after initial hemodynamic stabilization and routine investigations, were subjected to upper GI endoscopy within 72 hours of bleed to determine the etiology. Criteria for acute upper gastrointestinal bleed and all technical terms like upper GI bleeding, continuous bleeding, rebleeding, hematemesis, melena, hematochezia, and severity of bleeding were defined according to the criteria of American Society of Gastrointestinal Endoscopists (ASGE).[
8] Data were analyzed using simple statistical mean, average, percentage and standard deviation. An extensive search from different journals and publications was done to analyze the causes of UGIB in different regions of India, and comparison was made between the present study and other studies on UGIB to evaluate the etiological and clinical spectrum of bleeding in different regions of India.
Results
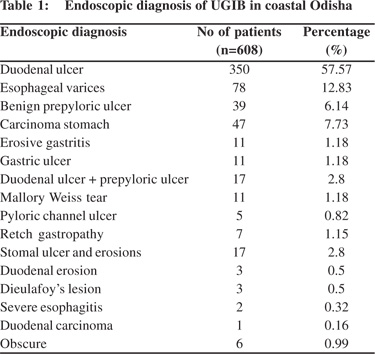
The study population comprised of 608 patients of UGIB from Odihsa. The majority were male (85.53%), and the male: female ratio was 6:1. The mean age of patients was 42+18.2 years. Melena was the presenting complaint in 95.06% (578/608) and hematemesis was present in 43.09% (262/608). Both hematemesis and melena were seen in 41.78% (254/608). Abdominal pain during the bleeding episode was seen in only 190 bleeders forming 31.25%, and the remaining 418 (68.75%) had painless bleed. History of NSAID intake was found in 46 patients (7.56%). Average episodes of bleeding in these patients were 2.09. Of the 608 bleeders 287 (47.2%) needed hospitalization and 210 (34.54%) required blood transfusions, while the majority i.e. 65.46% (398/608) did not required blood transfusion. The endoscopic diagnoses of the UGIB cases have been shown in Table 1. The commonest cause of UGIB was duodenal ulcer (DU), accounting for 57.6% cases. Variceal bleeding was responsible for bleed in only 12.8%. Benign pre-pyloric ulcer accounted for 6.4% cases; combined DU and benign pyloric ulcer for 3.6% and gastric ulcer for 1.8%. Neoplasms comprised 7.7% of cases. Other less common causes were erosive gastritis (1.8%), Mallory Weiss tear (1.8%), and retch gastropathy (1.1%). Curiously, of the patients with duodenal ulcer, only 54 out of 350 (15.4%) complained of pain during the bleeding episode.
 Discussion
Discussion
Upper gastrointestinal bleeding (UGIB) is a significant and potentially life-threatening worldwide problem.[
2] Despite advances in diagnosis and treatment, mortality and morbidity have remained more or less constant.2 Bleeding from the upper gastrointestinal tract (GIT) is about 4 times as common as bleeding from the lower GIT.[
2,
3] There are limited studies on UGIB from India. This study was undertaken to evaluate the etiology of UGIB in costal Odisha and to compare the results with studies from other parts of India.
Despite many advances like celiac/mesenteric angiography, push enteroscopy, 99Tc RBC scan and intraoperative enteroscopy to diagnose the cause of UGIB, upper gastrointestinal endoscopy (UGIE) remains the primary modality of evaluation. The diagnostic yield of UGIE is superior to that of barium studies. Endoscopy has a sensitivity of 92% when the entire stomach and proximal duodenum can be carefully visualized, and specificity that approaches 100%; by comparison barium radiography has a sensitivity of only 54%.[
15] Upper GI endoscopy was the reasonable option used to diagnose the cause of UGIB in the present study.
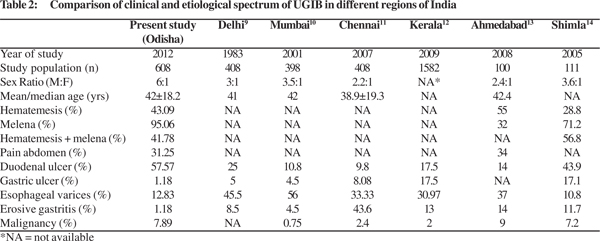
Table 2 compares the patient profile of UGIB from different parts of India; evidently there is great variation. There was a greater male preponderance in our study compared to ther studies on UGIB from different regions of India. The mean age of presentation (40-42 years) however, was comparable. Melena was the most common presentation in our study (95.06%) as compared to the study by Lakhani et al[
13] from Ahmedabad where hematemesis was the more common presentation (55%). Most of our patients presented with painless bleeding. In our study bleeding duodenal ulcer was the commonest cause of UGIB. This might be due to the greater prevalence of duodenal ulcer in Odisha.[
16] Variceal bleeding due to portal hypertension accounted for only a minority of cases (12.83%). This is in stark contrast to the reported spectra from Northern and Western India that create the impression that variceal bleeding is the most common cause of UGIB in India. This difference may be due to the fact that studies, which portray variceal bleeding as the commonest cause of UGIB, reflect severe cases that need urgent hospitalization. Besides, data from the All India Institute of Medical Science (AIIMS) are skewed because it is a major referral center for portal hypertension surgery, and hence cases of variceal bleeding from all over the country are referred to AIIMS. These figures are thus not representative of the actual etiological spectrum of UGIB in this country. The present study shows that duodenal ulcer is the commonest cause of upper gastrointestinal hemorrhage in coastal Odisha. Variceal bleeding accounted for barely one eighth of UGIB. Another interesting fact observed in the present study was that most patients of duodenal ulcer bleedsurprisingly presented with a painless bleeding episode. This should be kept in mind while evaluating a patient with UGIB.
 References
1
References
1. Ghosh S, Watts D, Kinnear M. Management of gastrointestinal haemorrhage. Postgrad Med J. 2002;78:4–14.
2. Rockall TA, Logan RFA, Devlin HB, Northfield TC. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. Steering Committee and members of the National Audit of Acute Upper astrointestinal Haemorrhage. BMJ 1995;311:222–6.
3. Hernandez-Diaz S, Rodriguez LA. Incidence of serious upper gastrointestinal bleeding/perforation in the general population: review of epidemiologic studies. J Clin Epidemiol. 2002;55:157–63.
4. Laine L, Peterson WL. Bleeding peptic ulcer. N Engl J Med. 1994;331:717–27.
5. Longstreth GF. Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1995;90:206–10.
6. Rockall TA, Logan RFA, Devlin HB, Northfield TC. Variation in outcome after acute upper gastrointestinal haemorrhage. The National Audit of Acute Upper Gastrointestinal Haemorrhage. Lancet. 1995;346:346–50
7. Bose D, Banerjee N, Sarangi B, Das S, Singh SP. Profile of upper gastrointestinal bleeding in a teaching hospital in coastal Orissa. Indian J Gastroenterol 1995;14(Suppl):A40.
8. Silverstain FE, Gilbert DA, Tedesco FJ, Buenger NK, Persing J. The national ASGE Survey on upper Gastrointestinal bleeding. II Clinical prognostic factors. Gastrointestinal Endosc. 1981;27:80–93
9. Anand CS, Tandon BN, Nundy S. The causes, management and outcome of upper gastrointestinal haemorrhage in an Indian hospital. Br J Surg. 1983;70:209–11.
10. Rathi P, Abraham P, Rajeev Jakareddy, Pai N. Spectrum of upper gastrointestinal bleeding in Western India. Indian J Gastroenterol 2001;20(suppl 2):A37.
11. Krishnakumar R, Padmanabhan P, Premkumar, Selvi C, Ramkumar, Joe A. Upper GI bleed- a study of 408 cases. Indian J Gastroenterol 2007;26(suppl 2):A133.
12. Gajendra O, Ponsek T, Varghese J, Sadasivan S, Nair P, Narayanan VA. Single center study of upper GI endoscopic findings in patients with overt and occult upper GI bleed. Indian J Gastroenterol 2009;28:A111.
13. Lakhani K, Mundhara S, Sinha R, Gamit Y, Sharma R. Clinical Profile of Acute Upper Gastro Intestinal Bleeding. Available at: http://www.japi.org/july_2008/gastro_enterology_hepatology [accessed 15 February 2012].
14. Kashyap R, Mahajan S, Sharma B, Jaret P, Patial RK, Rana S, Pal LS. A Clinical Profile of Acute Upper Gastrointestinal Bleeding at Moderate Altitude. JIACM 2005;6:224–8.
15. Dooley CP, Larson AW, Stace NH, Renner IG, Valenzuela JE, Eliasoph J, et al. Double-contrast barium meal and upper gastrointestinal endoscopy. A comparative study. Ann Intern Med 1984;101:538–45.
16. Tovey FI, Hobseley M, Kaushik SP, Pandey R, Kurian G, Singh K, et al. Duodenal gastric metaplasia and Helicobacter pylori infection in high and low prevalent areas in India. J Gastroenterol Hepatol 2004;19:497–505.