D. Muduly1, S.V.S. Deo1, N.K. Shukla1, N.M.L. Manjunath1, P. Durgapal2, A. Kallianpur1
Department of Surgical Oncology1, Dr BRA-IRCH and
Department of Pathology,2 All India Institute of Medical
Sciences, New Delhi, India 110029
Corresponding Author:
Dr. D. K. Muduly
Email: dillipmuduly@gmail.com
48uep6bbphidvals|564 48uep6bbph|2000F98CTab_Articles|Fulltext Inflammatory myofibroblastic tumor (IMT) is a very rare low grade malignant tumor with a potential to arise from any organ. Histologically, there is fibrous tissue proliferation without atypia in a back ground of chronic inflammatory cells. Although many hypothesis exist; neoplastic, infectious, reparative, or immunologic, the true etiology of IMT is unclear.[1,2] IMT of gall bladder is very rare. Only four case reports of IMT of gall bladder are available in literature.[3-6] We report a case of IMT of gall bladder in a patient with suspected cancer of gall bladder, who underwent radical cholecystectomy for gall bladder mass lesion.
Case Report
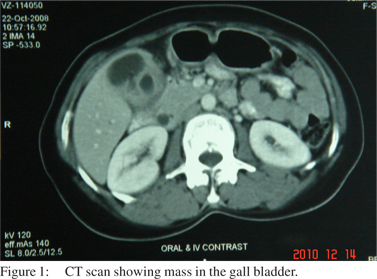
A 35 year old premenopausal woman presented to the hospital with history of low grade fever (on and off) and dull aching, irregular pain in right hypochondrium (unrelated to food) with occasional radiation to the back and right shoulder since 3 years. On clinical examination, gall bladder was palpable, smooth, firm with rounded margins and moving with respiration. Her hemoglobin was 10.7 gm/dl, serum bilirubin 0.6 mg/dl, AST 32 IU/L, ALT 28 IU/L, ALP 199 IU/L, albumin 4.6 gm/dl. Ultrasonography of the abdomen showed a mass lesion in fundus with a single large stone in gall bladder. Contrast enhanced computed tomography of abdomen and pelvis (Figure 1) revealed a mass lesion in the fundus of gall bladder. The plane with segment V of liver was ill defined with doubtful invasion of second part of duodenum. There were no significant lymph nodes along the hepatoduodenal ligament, peripancreatic, retroduodenal or celiac axis. She was a resident of Ganga river belt in northern India, which is a high risk region for carcinoma of gall bladder.[7] With the above history, clinical findings and imaging, a clinical diagnosis of carcinoma gal bladder was made.
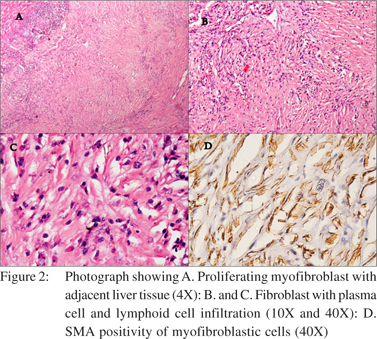
A radical cholecystectomy was performed with en-bloc resection of segment IVB and V of liver and periportal, retropancreatic and retroduodenal lymphadenectomy. Intraoperatively, there was a mass in the fundus of gall bladder with involvement of segment V of liver. Postoperative recovery was uneventful. On gross examination, the cut section showed a grayish white tumor from the fundus of gall bladder, which on histopathological examination showed spindle cell proliferation without atypia in a back ground of plasma cells and lymphocytes. The spindle cells expressed smooth muscle antigen (SMA) on immunohistochemical staining suggestive of cells of myofibroblastic origin. The tumor was reaching up to the capsule of liver without invasion (Figure 2A-D). She was discharged from hospital on post-operative day 5. She is on regular follow up and disease free since last 2 years.
 Discussion
IMT is a rare slow growing tumor with a potential to arise from many organs.[1] It has been variously named by different authors as inflammatory granuloma, inflammatory histiocytoma, plasmocytoma, plasma cell granuloma, pseudolymphoma and fibroxanthoma.[2] IMT was first described by Brunn in 1939.[3] and because of its resemblance to malignancy, it was named as “Inflammatory pseudotumor” by Umiker et al in 1954.[4] Earlier IMT was considered as non-neoplastic, but is currently considered as a tumor with low-grade malignant potential because of local recurrence, infiltrative growth pattern, vascular invasion and malignant transformation.[5]
Discussion
IMT is a rare slow growing tumor with a potential to arise from many organs.[1] It has been variously named by different authors as inflammatory granuloma, inflammatory histiocytoma, plasmocytoma, plasma cell granuloma, pseudolymphoma and fibroxanthoma.[2] IMT was first described by Brunn in 1939.[3] and because of its resemblance to malignancy, it was named as “Inflammatory pseudotumor” by Umiker et al in 1954.[4] Earlier IMT was considered as non-neoplastic, but is currently considered as a tumor with low-grade malignant potential because of local recurrence, infiltrative growth pattern, vascular invasion and malignant transformation.[5]
IMTs are rare tumors of undefined origin. Exact etiology is not known, although infection with inflammation has been proposed to be a causative factor. The new designation of ‘‘inflammatory myofibroblastic tumor’’ has replaced the earlier nomenclature of ‘‘inflammatory pseudotumor,’’ because the cell of origin was established as a myofibroblast by immunohistochemical markers and electron microscopic studies.[5] Although, most commonly occur in the lung[6], IMT can occur in any organ. They have been reported in liver, orbit, brain, spinal cord, lymph nodes, breast, thyroid gland, spleen, oesophagus, stomach, pancreas, gallbladder, retroperitoneum, ovaries, urinary bladder, kidney and larynx. Although IMT of liver and biliary tract is uncommon, liver is the most common site of hepatobiliary IMT.[3]
Nonsurgical interventions have also been described in literature for IMT of lung and liver in patients with preoperative histological diagnosis of IMT. These patients can be observed with close and regular follow-up until the condition resolves by itself or needed any further intervention.[7] There are case reports of complete resolution of the disease with steroids and NSAIDs.[8] There are no case reports of IMT of gall bladder being treated by conservative means. Malignant transformations and recurrences of IMT have been reported to occur between four to seven years after surgery.[1,9]Therefore, long-term follow up is necessary even for patients who have been successfully treated by surgical resection. The current case is disease free at 2 years after surgery. Few case reports are described in literature regarding metastatic potential of IMTs.[10] Whether the recurrences were true metastasis and how the authors have differentiated from second primary lesions or multifocal disease has not been described in these reports. Lifelong follow up is necessary even in patients with radical surgery, as the exact biological behavior of IMT is unknown.
References
- Hagenstad CT, Kilpatrick SE, Pettenati MJ, Savage PD. Inflammatory myofibroblastic tumor with bone marrow involvement. A case report and review of the literature. Arch Pathol Lab Med. 2003;127:865–7.
- Shek TW, Ng IO, Chan KW. Inflammatory pseudotumor of the liver. Report of four cases and review of literature. Am J Surg Pathol. 1993;17:231–8.
- Narla LD, Newman B, Spottswood SS, Narla S, Kolli R. Inflammatory pseudotumor. RadioGraphics. 2003;23:719–29.
- Umiker WO, Iverson L. Postinflammatory tumors of the lung; report of four cases simulating xanthoma, fibroma, or plasma cell tumor. J Thorac Surg. 1954;28:55–63.
- Coffin CM, Humphrey PA, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor: a clinical and pathological survey. Semin Diagn Pathol. 1998;15:85–101.
- Zennaro H, Laurent F, Vergier B, Rauturier JF, Airaud JY, Jougon J, et al. Inflammatory myofibroblastic tumor of the lung (inflammatory pseudotumor): uncommon cause of solitary pulmonary nodule. Eur. Radiol. 1999;9:1205–7.
- Koea JB, Broadhurst GW, Rodgers MS, McCall JL. Inflammatory pseudotumor of the liver: demographics, diagnosis, and the case for nonoperative management. J Am Coll Surg. 2003;196:226–35.
- Vassiliadis T, Vougiouklis N, Patsiaoura K, Mpoumponaris A, Nikolaidis N, Giouleme O, et al. Inflammatory pseudotumor of the liver successfully treated with nonsteroidal antiinflammatory drugs: a challenge diagnosis for one not so rare entity. Eur J Gastroenterol Hepatol. 2007;19:1016–20.
- Pecorella I, Ciardi A, Memeo L, Trombetta G, de Quarto A, de Simone P, et al. Inflammatory pseudotumour of the liver—evidence for malignant transformation. Pathol Res Pract. 1999;195:115–20.
- Kuo PH, Spooner S, Deol P, Monchamp T. Metastatic inflammatory myofibroblastic tumor imaged by PET/CT. Clin Nucl Med. 2006;31:106–8.
|