Sameer Vyas1, Ashish Khandelwal1, Manavjeet S Sandhu1, Subhash Verma2, Niranjan Khandelwal1
Department of Radiodiagnosis1 and Internal Medicine2
PGIMER, Postgraduate Institute of Medical Education and
Research, Chandigarh, India.
Corresponding Author:
Dr. Sameer Vyas,
E mail: sameer574@yahoo.co.in
48uep6bbphidvals|560 48uep6bbph|2000F98CTab_Articles|Fulltext Heterotopic pancreas (HP) is an uncommon entity. It is usually detected incidentally and may or may not be associated with complications related to the pathologic conditions of the pancreas itself but may present with complications like inflammation, bleeding, obstruction or malignant transformation.[1,2] HP in the mesentery of the small intestine is very rare. A brief review of the HP is discussed along with the case.
Case Report
A 19-year-old male presented with pain abdomen, fever and easy fatigability since one month. He had history of rheumatic heart disease with mitral and aortic regurgitation. The physical examination showed shifting dullness suggestive of free fluid in abdomen. The abdomen was soft and non-tender with no palpable mass and normal bowel sounds. Stools test was negative for occult blood. Hematologic examination and blood biochemical findings were normal as well except mildly deranged liver function. Ultrasonography revealed hepatosplenomegaly, bilateral medical renal disease, pleural and pericardial effusion. Contrast enhanced computed tomography (CECT) performed revealed similar findings and in addition showed the soft tissue in the small bowel mesentery which was distinctly separate from the pancreas proper, and showing homogeneous enhancement similar to pancreas without evidence of necrosis suggestive of HP (Figure 1). For exact confirmation of nature of lesion detected on CT, MRI was performed on 3Tesla MR system (Magnetom Verio, Siemens Medical Systems, Erlangen, Germany) with a phased-array body coil.T1-weighted imaging with and without fat suppression, and fat suppressed T2- weighted axial images revealed lobulated homogenous lesion in the mesentery with signal character similar to pancreas on all sequences (Figure 2).
Discussion
Heterotopic (ectopic, aberrant, accessory rest) pancreas is defined as the presence of pancreatic tissue, outside its usual location without any anatomical and vascular continuity with the normal pancreas proper.[1,2] It has a genetic make-up, physiologic function, and local environmental exposure similar to that of the pancreas. Heterotopic pancreatic tissue is often found incidentally in patients operated on for other reasons or during autopsies. Its frequency has been estimated as 1 case per 500 explorations of the upper abdomen or 0.6- 13.7% of autopsies.[3,4] It can present at any age but most commonly encountered in the 4th to 6th decades, and has a male preponderance.[1,2] The most frequent location of HP is the stomach (47%), followed by jejunum (35%), duodenum (11.7%) and ileum (5.8%).[3-6] The histological layers involved are, in descending order of frequency, the submucosa, muscularis propria, and serosa.[6] Other locations include the gallbladder, bile ducts, splenic hilum, umbilicus, fallopian tubes, mediastinum, esophagus, lymph nodes, omentum and meckel’s diverticulum.[6] The mesenteric location of HP is rare and there are only a few reported cases of HP in the mesentery of the small intestine.[6] The differential diagnosis of HP includes gastrointestinal stromal tumor, gastrointestinal autonomic nerve tumor , carcinoid, lymphoma, or even adenocarcinoma. HP is the second most common pancreatic congenital anomaly after divisum. It is postulated that early in fetal life, during rotation of the foregut and fusion of the dorsal and ventral parts of the pancreas, small parts are separated from it, and continue to develop in the wrong location. Histologically, the aberrant pancreatic tissue may contain all elements of normal pancreatic tissue such as acini, ducts and islet cells. The most characteristic gross feature is a central ductal orifice. Only about one-third of the patients with HP are symptomatic; frequent symptoms and signs are epigastric pain, abdominal fullness, tarry stools, vomiting, and diarrhea. Symptoms depend upon the anatomical location and its mass effect, such as gastric outlet obstruction in a pre-pyloric rest or obstructive jaundice in a bile duct focus and are also related to the size of the lesion.
Lesions greater than 1.5cm in diameter are more likely to cause symptoms. Complications related to the pancreas may be inflammation, cyst or pseudocyst formation, abnormal hormone secretion and malignant degeneration. In addition, complications unrelated to the pancreas may be gastric outlet, intestinal or common bile duct obstruction, intussusceptions or bleeding. Mesenteric heterotopic pancreatitis is a rare cause of acute abdominal pain.[6]
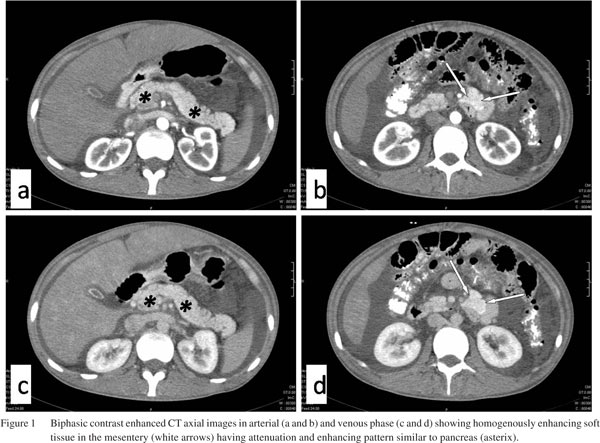
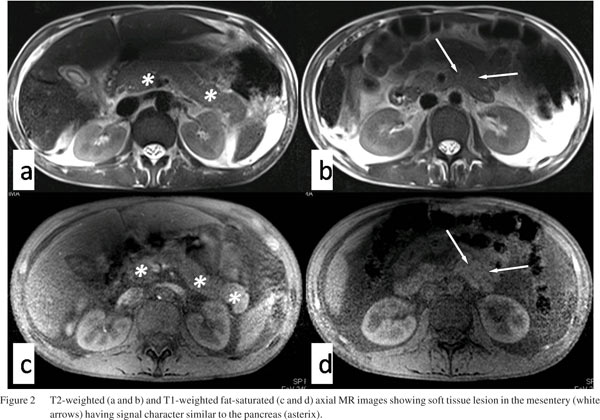 Different imaging modalities can be used to detect HP. Abdominal USG may be normal or show a cystic or heterogeneous mass in different parts of the abdomen.[7] In our case USG evaluation was limited for HP due to obscuration by bowel gases. The classic finding on radiographic barium study or at endoscopic examination is a submucosal mass with central umbilication.[6] CT findings are usually non specific. However, multi-detector CT with oral and intravenous contrast may demonstrate the lesion which enhances similarly with the normal pancreatic tissue as seen in our case. The appearance and enhancement pattern of HP on CT scans have been reported to be unreliable in differentiating the condition from gastrointestinal stromal tumor or carcinoid tumor. Visualization of the duct with MRCP was diagnostic of HP, obviating histologic confirmation in cases previously described.6 In our case duct was poorely visualised due to non dilatation and absence of any pathology affecting it.
The combination of endoscopic ultrasonography with fineneedle aspiration cytology has been used for evaluation of submucosal gastrointestinal lesions. Preoperative biopsy may not help in the diagnosis of HP, and except for a few cases, definitive diagnosis of HP was not established preoperatively even in the symptomatic patients. Both conservative treatment and follow-up or removal of HP to prevent future complications is the recommended treatment options. Resection of the ectopic rest is advisable when the condition is encountered coincidentally during the operation.
In conclusion, HP in mesentery is extremely rare and imaging diagnosis of this condition is hardly described previously especially in asymptomatic patients. Signs and symptoms of the disease may cause confusion in the clinical diagnosis, if the pathologic conditions develop in the heterotopic tissue. However, the characteristic imaging features of HP may help in establishing the diagnosis.
Different imaging modalities can be used to detect HP. Abdominal USG may be normal or show a cystic or heterogeneous mass in different parts of the abdomen.[7] In our case USG evaluation was limited for HP due to obscuration by bowel gases. The classic finding on radiographic barium study or at endoscopic examination is a submucosal mass with central umbilication.[6] CT findings are usually non specific. However, multi-detector CT with oral and intravenous contrast may demonstrate the lesion which enhances similarly with the normal pancreatic tissue as seen in our case. The appearance and enhancement pattern of HP on CT scans have been reported to be unreliable in differentiating the condition from gastrointestinal stromal tumor or carcinoid tumor. Visualization of the duct with MRCP was diagnostic of HP, obviating histologic confirmation in cases previously described.6 In our case duct was poorely visualised due to non dilatation and absence of any pathology affecting it.
The combination of endoscopic ultrasonography with fineneedle aspiration cytology has been used for evaluation of submucosal gastrointestinal lesions. Preoperative biopsy may not help in the diagnosis of HP, and except for a few cases, definitive diagnosis of HP was not established preoperatively even in the symptomatic patients. Both conservative treatment and follow-up or removal of HP to prevent future complications is the recommended treatment options. Resection of the ectopic rest is advisable when the condition is encountered coincidentally during the operation.
In conclusion, HP in mesentery is extremely rare and imaging diagnosis of this condition is hardly described previously especially in asymptomatic patients. Signs and symptoms of the disease may cause confusion in the clinical diagnosis, if the pathologic conditions develop in the heterotopic tissue. However, the characteristic imaging features of HP may help in establishing the diagnosis.
References
- Agale SV, Agale VG, Zode RR, Grover S, Joshi S. Heterotopic pancreas involving stomach and duodenum. J Assoc Physicians India. 2009;57:653–7.
- Yuan Z, Chen J, Zheng Q, Huang XY, Yang Z, Tang J. Heterotopic pancreas in the gastrointestinal tract. World J Gastroenterol. 2009;15:3701–3.
- De Castro Barbosa JJ, Dockerty MB. Pancreatic heterotopia: review of the literature and report of 41 authenticated surgical cases, of which 25 were clinically significant. Surg Gynecol Obstet. 1946;82:527–42.
- Dolan RV, ReMine WH, Dockerty MB. The fate of heterotopic pancreatic tissue: a study of 212 cases. Arch Surg. 1974;109:762–5.
- Lai EC, Tompkins RK. Heterotopic pancreas: review of a 26 year experience. Am J Surg. 1986;151:697–700.
- Silva AC, Charles JC, Kimery BD, Wood JP, Liu PT. MR Cholangiopancreatography in the detection of symptomatic ectopic pancreatitis in the small-bowel mesentery. AJR Am J Roentgenol. 2006;2:W195–7.
- Henry C, Prot T, Maitre S, et al. A rare cause of acute abdominal pain: mesenteric heterotopic pancreas complicated by acute pancreatitis. Gastroenterol Clin Biol. 2000;24:370–1.
|