48uep6bbphidvals|429
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Infarction of the greater omentum is a rare cause of acute
abdomen with only few cases reported in the literature. Given its low incidence and lack of awareness among clinicians, an
accurate preoperative diagnosis is unusual and patients may be explored for peritonitis due to other causes. Omental
gangrene presenting as a late complication following corrosive ingestion has not been reported in the literature. To our
knowledge we report here the first case of omental gangrene occurring nearly three months after corrosive ingestion,
presenting as an acute abdomen and requiring surgery.
Case Report
A 40-year old female had ingested corrosive acid 3 months
ago, following which she developed abdominal pain associated with vomiting and was managed conservatively. She had no
respiratory distress, hemoptysis or hematemesis. She developed dysphagia to solids and semisolids 1 month later.
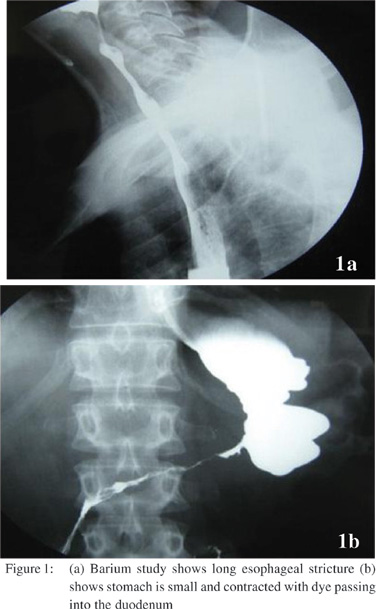
Barium study showed a long esophageal stricture (Figure 1a) with a small capacity contracted stomach, and passage of dyeinto the duodenum (Figure 1b). She was planned for an upper gastrointestinal endoscopy and possible dilatation of
esophageal stricture. Esophagoscopy revealed a stricture just
below the upper esophageal sphincter for which dilatation was
attempted. A day after dilatation, patient came with acute onset
severe pain abdomen.On examination her pulse rate was 120/
min and BP 100/60 mmHg. Abdominal examination showed signs
of peritonitis. She was resuscitated with intravenous fluids
and intravenous antibiotics were started. Blood gases showed
metabolic acidosis. With a pre-operative suspicion of lower
esophageal perforation, the patient underwent exploratory
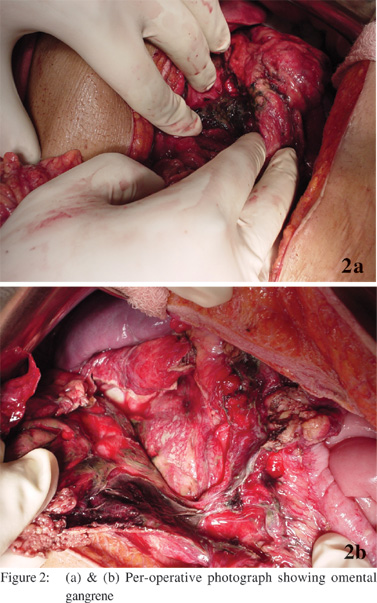
laparotomy. Per operative findings revealed dark hemorrhagic
foul smelling fluid with gangrenous omentum (Figures 2a & 2b) and no evidence of gastric or esophageal perforation. Stomach was small and contracted. Surgical procedure included
omentectomy, feeding jejunostomy, lavage and drainage. She
was kept on elective ventilation and was extubated after her
acidosis was corrected. Postoperatively she developed chest
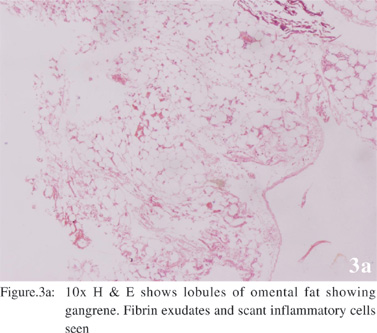
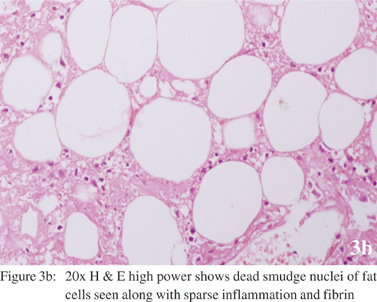
infection which was treated with antibiotics. She wasdischarged after 2 weeks. Histopathology showed lobule of
omental fat showing gangrene with fibrin exudates and few
inflammatory cells (Figures 3a & 3b). At 3-months follow up she is taking feed through jejunostomy and is being worked
up for definitive surgery.
Discussion
Primary omental torsion was first reported by Eitel in 1899 in
which a bulky and mobile greater omentum particularly on the right side twists around the distal right epiploic vessels with
subsequent venous occlusion, edema and arterial thrombosis leading to gangrene. Johnson[1] in 1932 first described, primary
omental infarction without torsion. The reported incidence is 0.1% of patients undergoing laparotomy for appendicitis.[2] The
incidence has been rising attributed to increased awareness of
the entity, technical advancements in imaging and utilization
of CT scan for evaluation of abdominal pain.
The exact etiology is not known. Predisposing factors
reported in the literature include variations in arterial supply to
the right side of the greater omentum, excess omental fat
associated with obesity (explaining its greater incidence in
adults), hypercoagulability, trauma, straining, vascular
congestion secondary to overeating, overexertion, and sudden
positional change.[3] Omental infarction in adults is rarely
described following intra-abdominal surgery, after marathon
running, with right-sided heart failure, or as a complication of
vasculitis[4].
To our knowledge this is the first case in which corrosive
ingestion has been the pathophysiological mechanism for the etiology of late omental infarction. The reason for late
development of omental gangrene following corrosive intake
is not known, but could possibly be related to the development
of thrombosis of the omental vessels resulting from inflamed contracted stomach following corrosive ingestion.
The right side of the omentum is affected in the majority of
patients leading to right sided abdominal pain. The right-sided predilection is usually attributed to anomalous right omental
vascular development.[5,6] It was predominantly left sided in our case, probably related to the etiology of gangrene. Other
symptoms include low grade fever and occasional vomiting. Leukocyte count may be mildly elevated.
Characteristic features[7,8] of omental infarction on imaging
may help in making a preoperative diagnosis in suspicious cases. The omental infarct on CT scan appears as an ovoid
area of high attenuated fat containing hyperattenuated streaks just beneath the parietal peritoneum with thickening of the
overlying anterior abdominal wall. Ultrasound scan shows the omental infarct typically appearing as a hyperechoic, noncompressible,
ovoid intra-abdominal mass adherent to the anterior abdominal wall with localized point tenderness.
Omental infarction usually follows a benign course that
allows conservative management. Spontaneous and complete
resolution of symptoms typically occurs within 2 weeks.
However non-operative treatment has a risk of leaving the
necrotic tissue inside, resulting in prolonged convalescence
due to gangrene or abscess formation. Omental abscess and
bowel obstruction are the delayed complications of omental
infarction.
Surgery is indicated in patients who have worsening of
symptoms on conservative management, in whom omental gangrene result in sepsis and when there is diagnostic dilemma.
Surgery usually results in early resolution of symptoms with little morbidity. Histology shows hemorrhagic infarction associated with fat necrosis, followed by cellular infiltration,
fibrosis and scar formation.
References
- Johnson AH. The great omentum and omental thrombosis.
Northwest Med. 1932;31:285–90.
- Lardies JM, Abente FC, Napolitano A, Sarotto L, Ferraina P.
Primary segmental infarction of the greater omentum: a rare cause
of RLQ syndrome; laparoscopic resection. Surg Laparosc Endosc
Percutan Tech. 2001;11:60–2.
- Rich RH, Filler RM. Segmental infarction of the greater omentum: a case of the acute abdomen in childhood. Can J Surg.
1983;26:241–3.
- Wiesner W, Kaplan V, Bongartz G. Omental infarction associated
with right-sided heart failure. Eur Radiol. 2000;10:1130–2.
- Ho CL, Devriendt H. Idiopathic segmental infarction of right sided greater omentum: Case report and review of the literature.
Acta Chir Belg. 2004;104:459–61.
- Mainzer RA, Simoes A. Primary idiopathic torsion of the omentum: Review of the literature and report of six cases. Arch
Surg. 1964;88:974–83.
- Puylaert JB. Right sided segmental infarction of the omentum:
clinical, US, and CT findings. Radiology. 1992;185:169–72.
- Karak PK, Millmond SH, Neumann D, Yamase HT, Ramsby G. Omental infarction: report of three cases and review of the
literature. Abdom Imaging. 1998;23:96–8.