48uep6bbphidvals|38
48uep6bbphidcol4|ID
48uep6bbph|2000F98CTab_Articles|Fulltext
The world over, liver transplantation has emerged a panacea for thousands of patients suffering from end-stage liver disease. More than 10,000 liver transplants are being performed all over the world every year. In the 1990s, it was estimated that annually more than 200,000 patients in India succumbed to terminal liver disease and its complications. Many of these patients might have been saved by well-planned liver transplantation, which was not available at the time. Lack of legal sanction for brain-stem death declaration, non-existent deceased organ donor system and lack of regulation for living donation were amongst the restrictions encountered. This realisation prompted the passing of the Human Organ Transplantation Act of 1994. This law was to have had furthered the availability of organs for transplantation and to have had conclusively put an end to the organ-trade racket. However, these hopes were belied.
EVOLUTION OF LIVER TRANSPLANTATION IN INDIA
After 2 unsuccessful attempts in 1995 and 1996, the first successful deceased donor liver transplant (DDLT) was performed in 1998. However, due to the sporadic availability of deceased donor organs, a patient requiring liver transplant would almost certainly die before an organ could become available. Liver transplantation remained a realistic option only for the few who could afford the astronomical costs of travelling overseas for the procedure.
In parallel with this, the art and science of hepatology and liver surgery had made rapid advance in both the understanding of the disease and its treatment. Liver resections, once associated with significant mortality had become safer, relatively bloodless and morbidity-free. After initial unsuccessful attempts in Brazil, the first successful living donor liver transplantation (LDLT) was performed in Australia from parent to child using the left lobe in 1989. This was followed by similar successful attempts in the United States. This was a brand new hope for children suffering from end-stage liver disease, who no longer had to wait for a reduced deceased donor liver to become available and the procedure was adopted with prodigious fervour all over the world. Taking cue from the success of left lobe transplants and employing their expertise in liver resections, Japanese surgeons pioneered adult-to-adult LDLT (AALDLT) using the right lobe in 1993. This was marked the world over, particularly in Asian countries where viral hepatitis was prevalent. This seemingly was the Holy Grail for meeting the ever-increasing demand for liver transplantation in countries where deceased donor livers were rarely available, as well as to bridge the demand-supply gap in other countries.With increasing experience, innovations like the modified right lobe graft, the extended right lobe graft, the right posterior sector graft, the left lobe (including the caudate lobe) graft and the dual graft have made it possible to provide adequate functional hepatic mass in any situation including high-urgency situations with a high degree of success and donor safety.
Many Indian hepatologists and surgeons who had received training in liver transplantation abroad were anxious to develop this specialty in India. It was estimated that almost 20,000 Indian patients needed liver transplants every year. The strides made in LDLT by Asian centres particularly in Japan, Korea, Hong Kong and Taiwan made many Indian centres realise that while efforts to promote donation of deceased donor organs had to continue, in order to sustain liver transplant activity in the country, a similar solution had to be found. This prompted many surgeons to visit these Asian centres for training in LDLT to equip them to start LDLT in their own centres.
The first successful LDLT in India was performed from an adult donor to a paediatric recipient in 1998. This was the prelude to establishing LDLT in India. It was followed by several procedures at select centres that met with mixed success. With these reports suggesting that the infrastructure and technical expertise could be made available with institutional support and resolve, many centres embarked on setting up or upgrading their resources to meet the demands of LDLT.
NEED AND FEASIBILITY OF LDLT IN INDIA
In India where historical and cultural issues have impeded the ready availability of cadaveric organs for donation, at least currently, LDLT is the only realistic option. Some of the inherent hurdles in DDLT include timely availability of a deceased donor organ before the patient becomes too sick to receive a transplant, organ harvesting and transport, likelihood of marginal grafts due to paucity of expertise in management of brain dead donors and difficulty for the recipient to arrive at the transplant centre at short notice. It is no wonder therefore, that more than 70% of the liver transplants performed in this country till date have been LDLTs.
Before assessing its feasibility in India, it is pertinent to define the pre-requisites for establishing an LDLT programme. Obviously the procedure is very resource intensive and requires skilled multidisciplinary manpower. It is however not imperative that the centre has experience in performing DDLT though such experience can be beneficial. At least two surgeons with significant experience in advanced hepatobiliary surgery and assistant surgeons are required per surgical team. The surgical team has to be actively supported by a group of highly skilled and experienced anaesthetists, critical care physicians and transplant hepatologists with a round-the-clock access to diagnostic and interventional radiology, dialysis, endoscopy, immunology, pathology, transfusion, microbiology and biochemistry services of the highest quality. At least two state of the art operating rooms equipped with rapid infusers, cell savers, non-invasive cardiac output monitors, ultrasonic surgical aspirator, argon coagulator and on-site laboratory are necessary. In the post-operative period, a modern intensive care facility with invasive monitoring, laminar flow and skilled nursing staff form the remaining links in the chain.
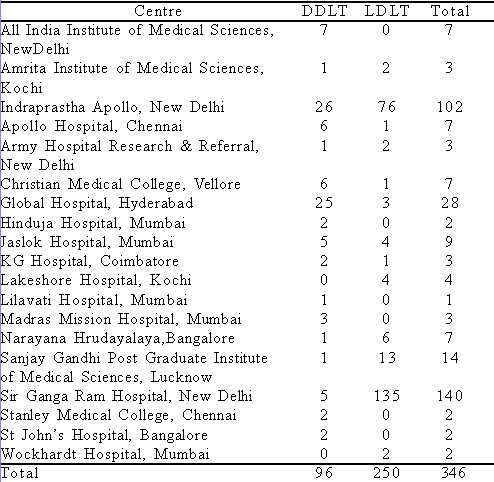
A total of 22 centres have performed liver transplants in this country, of which 14 have performed at least one LDLT procedure with success ranging from 0–92%, according to a recent survey by our group (Table I).(1)2 centres, including our own have performed more that 50 LDLTs since the beginning of their respective programmes. From the numbers heavily skewed towards LDLT, it is evident that most of these patients and perhaps all those requiring emergency liver transplants would not have survived without LDLT.
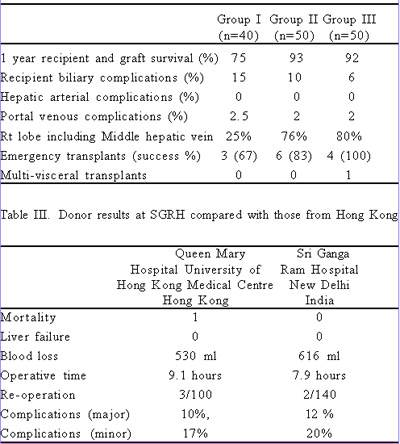
At the time of writing this we have performed 140 LDLT procedures at our centre of which 13 have been performed in emergency circumstances. While we encountered many problems during the initial experience, our current patient and graft survival rates (92% for the last 100 cases) compare with the best reported.(2,3) In that context, it is useful to follow the results as they evolved in our programme. Table II provides the details of recipient morbidity and mortality in our series divided into 3 successive cohorts comprising first 40, next 50 and last 50 transplants. Our programme has evolved and we now perform LDLT in high-risk groups such as infants, the elderly, those with fulminant hepatic failure, renal dysfunction, portal vein thrombosis, and in those requiring simultaneous liver and kidney transplants. We have introduced several innovations along the way to avoid anterior sector congestion of the right lobe, reduce biliary complications and utilise small grafts or those with difficult vascular and biliary variations.
There have been no donor deaths. The donor morbidity has been similar to that reported elsewhere(4,5) (Table III). Our results clearly demonstrate that LDLT is feasible in India even in emergency situations.
BENEFITS OF LDLT
The success of the procedure at large capacity centres in Korea, Hong Kong and Japan bears testimony to the benefit of LDLT in a significant number of patients with terminal liver disease in those countries. Even in countries where the DDLT is active, LDLT is making significant inroads by reducing mortality of patients on waiting lists. The number of cases at our centre has been rising continuously since the inception of the programme, increasing to the present figure of around 90– 100 transplants a year. Countrywide, even 10–15 such centres would significantly benefit a large number of suffering patients. LDLT has certain other advantages. It allows for adequate preparation of the patient for elective transplant. In addition, since the live donation is targeted, these recipients are not in competition with others over the same donor organ. Hence, LDLT is possible for many patients with borderline indications for DDLT such as those with hepatomas beyond Milan criteria, HIV, recurrent HCV disease and ethanol related acute-on-chronic liver failure with less than 6 months abstinence.
The other advantages of LDLT are complete screening of the donor organ before use and short ischaemic time probably resulting in a better quality graft provided small-for-size dysfunction is avoided. In fact, there are reports that in the last 5 years, LDLT has yielded better results than DDLT.(6)
As transplant clinicians in India, we must continue our endeavour to make liver transplantation as successful and as widely accessible as it is in the West. Widespread but carefully regulated use of LDLT is likely to help in both. A proportional increase in success rate with increasing number of operations has been noted in most complex surgical procedures.(7) Our experience with LDLT suggests the same (Table II). As more patients undergo successful transplantation, awareness and confidence in this procedure will increase, furthering its growth. Spread of awareness of the success of liver transplantation (LDLT) is likely to favourably influence societal perception about the importance of organ donation by deceased donors. The fair share of media attention received by the recent success of LDLT, will help us in achieving this. It is hoped that this will increase awareness of liver disease, liver transplantation and organ donation that may ultimately result in a more receptive audience for organ donation and will see increased donation rates like in certain Asian countries.
DISADVANTAGES OF LDLT
An omnipresent concern with LDLT is one of donor safety particularly with the right lobe graft and the extended right lobe graft. While a donor major complication rate of approximately 1% is routinely stated, unconfirmed reports suggest that the actual rates may be higher. There have been reports of at least two living donor deaths in India whilst the actual morbidity of the procedure is unreported. Recent reports of donor mortality from well-established Asian centres where the procedure has been performed for several years further reinforce the maxim that no amount of attention to donor safety is excessive. Hence, the centre must be entirely equipped in terms of infrastructure and multidisciplinary expertise before embarking on an LDLT programme. In addition, details and results of all operations must be entered in a National/State Registry as well as audited internally and at the Governmental level.
Apart from donor risk, the only aspect where DDLT reportedly scores over LDLT today appears to be a slightly lower risk of biliary complications. However, our experience has been different. Since most centres report a similar incidence of arterial complications in the two settings, the higher rate of biliary complications in LDLT is likely technical or maybe attributed to the cut surface rather than related to ductal ischemia. We have shown (paper submitted for presentation at the 2007 Congress of the European Society of Transplantation) that with certain technical modifications, the biliary complication rate in LDLT can be brought down to less than 10%, which is similar to that reported in DDLT.(8)
The cost of LDLT is significant, varying between10 and 20 lakh rupees in this country. This is one reason why it has mostly been confined to the private sector. Indigenisation of materials, support by medical insurance and welfare schemes are likely to significantly reduce costs and make the procedure more affordable.
CONCLUSION
In conclusion, as shown in Sri Ganga Ram Hospital (currently performing 8 transplants a month), establishing a high volume LDLT centre with excellent success rates is feasible in the Indian setting. While no efforts should be spared to promote deceased donor organ availability, LDLT has become a necessary supplement to DDLT in India. It is also required to promote public acceptance of liver transplantation. It might even help in promoting deceased donor organ donation. However, it is necessary to adopt an extremely cautious attitude so as to prevent unregulated proliferation of LDLT centres. Strict adherence to and fostering of internationally accepted norms of training and set-up as well as internal and external auditing of results must be made compulsory before permitting centres to carry out LDLT. In particular, the living donor must be protected under all circumstances if continuing clinical benefits are to be reaped from LDLT.
REFERENCES
1. Kakodkar R, Soin AS, Nundy S. Liver Transplantation in India: its evolution, problems and the way forward. Natl Med J India. 2007;20:53–6.
2. Liu CL, Fan ST. Adult-to-adult live-donor liver transplantation: the current status. J Hepatobiliary Pancreat Surg. 2006;13:110–6.
3. Morioka D, Egawa H, Kasahara M, Ito T, Haga H, Takada Y et al. Outcomes of adult-to-adult living donor liver transplantation: a single institution’s experience with 335 consecutive cases. Ann Surg. 2007;245:315–25.
4. Chan SC, Fan ST, Lo CM, Liu CL, Wong J. Toward current standards of donor right hepatectomy for adult-to-adult live donor liver transplantation through the experience of 200 cases. Ann Surg. 2007;245:110–7.
5. Lo CM, Fan ST, Liu CL, Yong BH, Wong Y, Lau GK et al. Lessons learned from one hundred right lobe living donor liver transplants. Ann Surg. 2004;240:151–8.
6. Maluf DG, Stravitz RT, Cotterell AH, Posner MP, Nakatsuka M, Sterling RK, et al. Adult living donor versus deceased donor liver transplantation: a 6-year single center experience. Am J Transplant. 2005;5:149–56.
7. Axelrod DA, Guidinger MK, McCullough KP, Leichtman AB, Punch JD, Merion RM. Association of center volume with outcome after liver and kidney transplantation. Am J Transplant. 2004;4:920–7.
8. Pascher A, Neuhaus P. Bile duct complications after liver transplantation. Transpl Int. 2005;18:627–42.