Introduction
Gastric outlet obstruction (GOO) is a clinical syndrome that can manifest with a variety of symptoms, including abdominal pain, postprandial vomiting, early satiety, and weight loss. It is caused by mechanical impediment to gastric emptying which can be at the distal stomach, pyloric channel, or duodenum1. The etiology of GOO is divided into benign or malignant. Until late 1970s, benign disease was responsible for majority of GOO in adults (of which peptic ulcer disease accounted for 90% of cases), while malignancy accounted for only 10 to 39 percent of cases2,3. With the decline in peptic ulcer disease, 50 to 80 percent cases of GOO are attributable to malignancy4-6. Even in a developing country like India, malignancy has been reported as the commonest cause of GOO6-8. Amongst malignant causes of GOO, gastric malignancy has been reported as the commonest cause in India6-8. Amongst benign causes of GOO, Misra et al.6 and Sukumar V et al8 has reported peptic ulcer disease as the commonest cause in India6,8. In contrast Maharshi S et al9 has reported that approximately equal proportions of benign GOO were due to corrosive injury; gastroduodenal tuberculosis and peptic ulcer disease.
There is paucity of data regarding etiological spectrum of GOO in India. There is no study available, from our region in Sub Himalayan Ranges of North India, regarding the etiological spectrum of GOO.
We therefore conducted this study to find out current trends in etiological spectrum of gastric outlet obstruction from our region.
Methods
In this study we did a retrospective review of the endoscopy registry data, which is maintained in the Department of Gastroenterology IGMC Shimla, a tertiary care hospital in the state of Himachal Pradesh in Sub Himalayan range of North India. Record of all patients above 18 years of age,who were diagnosed to have gastric outlet obstruction on endoscopy from January 2016 to December 2021 were reviewed. Patients in whom a senior gastroenterologist was unable to negotiate the standard gastroscope (Olympus EXERA II GIF-H180) across the pylorus into the distal duodenum (D3 –third part) due to mechanical impediment were considered to have GOO and were included in the study.
Records of the histopathology reports of the tissue specimens obtained from obstructing area were reviewed for confirmation of the etiology of GOO. Patients of peptic ulcer disease with GOO were included when their obstruction failed to improve with medical therapy (including anti H pylori and proton pump inhibitors therapy). The diagnosis of gastroduodenal TB was made on the basis of pathological lesions in the antrum, pylorus or duodenum showing presence of epitheloid granulomas, acid fast bacilli (AFB) on Ziehl Neilson staining or polymerase chain reaction (PCR) positivity for Mycobacterium TB on endoscopic biopsies and clinical response to anti-tubercular therapy (ATT). The diagnosis of corrosive GOO was based on a history of corrosive ingestion with evidence of injury on endoscopy. Patients with gastroparesis without any mechanical obstruction and previous diagnosis of malignancy were excluded from the study.
The data analyzed included age, gender, endoscopic findings and histopathology reports of the included patients. The objective of the study was to find out the various etiologies that lead to GOO. Our study was approved by the institutional ethics committee.
Statistical Analysis
Statistical analysis was performed using statistical package for social sciences (SPSS) version 22.0 for Windows (SPSS, Chicago, IL, USA). Results are displayed in tables and figures, with the categorical variables presented as numbers and percentages and mean ± standard deviation (SD), as appropriate. Unpaired T-test was used to compare the characteristics of malignant and benign etiologies of GOO.
Results
During the study period from January 2016 to December 2021, a total of 421 patients were diagnosed to have gastric outlet obstruction (GOO) and were included in the study. The mean age of the study population was 56.9±14.1 years [Table 1].
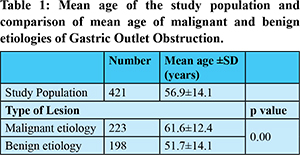
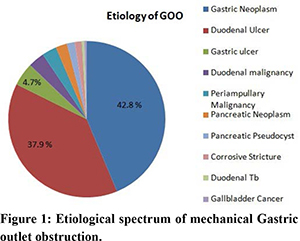
Majority of the patients (87.4%) were above the age of 40 years [Table 2]. Three hundred twelve of the 421 (74.1%) patients were male, with male to female ratio of 2.8:1.0 [Table 2]. Malignant etiology for GOO was more common and is seen in 223 (53%) cases as compared to benign etiology seen in 198 (47%) cases. The mean age (61.6±12.4 years) of the malignant etiology of GOO was statistically significant when compared with the mean age (51.8±14.1 years) of the benign etiology of GOO [Table 1]. Overall gastric malignancy (42.8%) was the most common etiology followed by duodenal ulcer (37.9%), benign gastric ulcer (4.7%), carcinoma duodenum (3.3%), periampullary carcinoma (3.0%), pancreatic malignancy (2.3%), extrinsic compression by pancreatic pseudocyst (1.6%), corrosive stricture (1.4%), duodenal tuberculosis (0.5%) and gallbladder cancer (0.5%) [Figure 1].
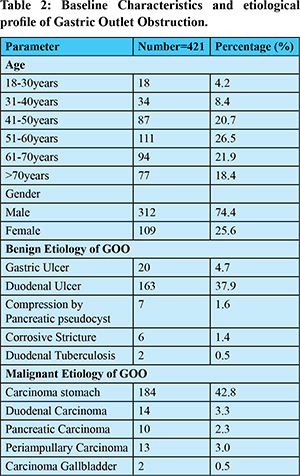
Gastric malignancy and peptic ulcer disease accounted for 85.4% of the all cases of GOO. Out of 184 cases of gastric malignancy, 175 (95.1%) were adenocarcinoma and 9 (4.9%) were diffuse large B- cell lymphoma. Gastric malignancy was the most common cause of malignant GOO while duodenal ulcer was the most common cause of the benign GOO [Table 2].
Age distribution with underlying etiology revealed duodenal ulcer to be the most common cause of the GOO from third to fifth decade followed by gastric malignancy [Table 3]. Among elderly patients from 6th decade onward gastric malignancy was the most common cause of GOO followed by duodenal ulcer [Table 3]. The gender distribution with underlying etiology revealed duodenal ulcer to be the most common cause of the GOO followed by gastric malignancy in males, while gastric malignancy followed by duodenal ulcer in females [Table 3].
Discussion
In the present study, most patients of GOO were males with male to female ratio of 2.8:1. Similar observations have been reported in previous studies with males outnumbering the females as cause of GOO6-10. Majority of the patients were in 5th, 6th, and 7th decade of life with mean age of 56.9±14.1 years. This finding was concurrent with previous study from south India in which the maximum numbers of patients were in their sixth and seventh decade with mean age of 59.79 ± 13.528. In a study by Misra et al. from North India, the mean age of the study population was 58±13 years, similar to our study6.
The study demonstrates that the predominant cause for GOO in Sub – Himalayan ranges of Northern India is malignant etiology (53%). This concurs with findings of Misra et al.6 from Northern India and Sukumar et al8 from Southern India, where malignancy was reported to cause GOO in 76% and 61.4% of the total cases respectively.
In our center gastric malignancy was the most common cause of GOO, and this was especially true for elderly patients. Gastric malignancy as most common cause of GOO has been reported in other studies from India6-8,11,12 [Table 4]. Pancreatic adenocarcinoma with extension to duodenum or stomach has been reported as a common cause of malignant GOO in western studies accounting for 15-25% of cases13. In our study pancreatic cancer was seen in only 2.3% of the cases and similar lower prevalence of pancreatic cancer as cause of GOO has been reported in other studies from India6,7,8,12 [Table 4].
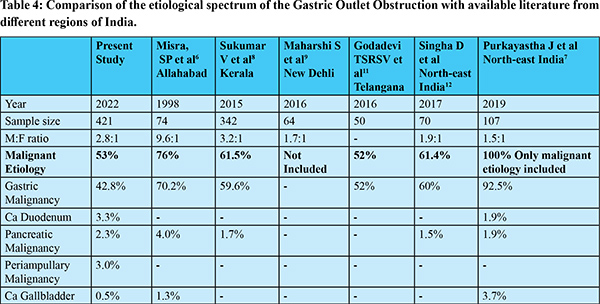
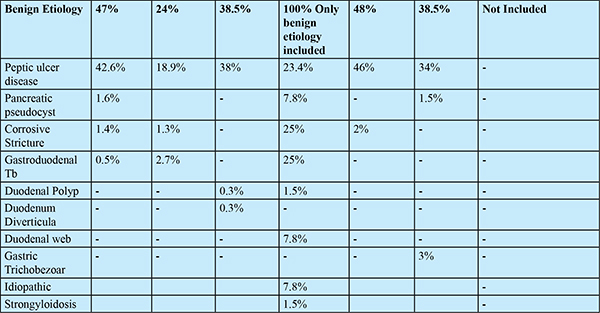
In our center peptic ulcer disease was the most common benign cause of GOO, and this was especially true for younger patients. Peptic ulcer disease is also the most common cause of acute upper gastrointestinal bleeding in our region which is in contrast to the reports from other centers of India (where portal hypertension related upper gastrointestinal bleeding is most common)14. Peptic ulcer disease as most common benign cause of GOO has also been reported in previous studies from India6,8,11,12. Other etiologies of benign GOO like extrinsic compression by pancreatic pseudocyst (1.6%), corrosive stricture (1.4%) and duodenal tuberculosis (0.5%) were less commonly seen in our patients. This is in accordance with the previous studies by Misra et al. from Northern India6 and Sukumar et al8 from Southern India but in contrast to the study by Maharshi et al from Northern India9. Maharshi et al9 in their study reported that approximately equal proportions of benign GOO were due to corrosive injury; gastroduodenal tuberculosis; and peptic ulcer disease. This contrast in etiology of benign GOO could represent either a true epidemiological difference or reflect skewed access to health care. It seems likely that the study conducted in the major referral centers of India may represent the referral bias in the etiological spectrum of GOO requiring endoscopic and surgical intervention which may have added on to the percentage of patients with refractory corrosive stricture and gastroduodenal tuberculosis.
Limitations
The present study is retrospective in nature and analyzed the age, sex and etiology of the endoscopically confirmed GOO. The study did not prospectively follow these patients to determine their future course. The surgeries or the endoscopic interventions these patients underwent were not followed. Among patients with GOO due to peptic ulcer disease, eradication of H. pylori could not be confirmed due to lack of facility for urea breath testing and fecal antigen testing in our center.
Conclusion
The etiology of GOO in Himachal Pradesh, Northern India is predominantly malignant (53.0%) but significant percentages (47%) also have benign causes. Overall gastric malignancy (42.8%) was the most common etiology followed by peptic ulcer disease (42.6%). Peptic ulcer disease was the most common cause of the GOO in younger age patients (from third to fifth decade) while carcinoma stomach was the most common cause of GOO among elderly patients (6th decade and above). Males were more commonly affected with GOO than females.
References
- Tringali A, Giannetti A, Adler DG. Endoscopic management of gastric outlet obstruction disease. Ann Gastroenterol. 2019; 32(4):330-337.
- Johnson CD. Gastric outlet obstruction malignant until proven otherwise. Am J Gastroenterol. 1995; 90:1740.
- Johnson, CD, Ellis, H. Gastric outlet obstruction now predicts malignancy. Br J Surg 1990; 77: 1023–1024.
- Chowdhury A, Dhali GK, Banerjee PK. Etiology of gastric outlet obstruction. Am J Gastroenterol. 1996; 91:1679.
- Shone DN, Nikoomanesh P, Smith-Meek MM, Bender JS. Malignancy is the most common cause of gastric outlet obstruction in the era of H2 blockers. Am J Gastroenterol. 1995;90:1769–70
- Misra SP, Dwivedi M, Misra V. Malignancy is the most common cause of gastric outlet obstruction even in a developing country. Endoscopy 1998; 30: 484–486.
- Purkayastha J, Bannoth S, Kalita D, Talukdar A, Borthakur BB, Pegu N, Das G. A Study of Clinical Presentation and Management of Malignant Gastric Outlet Obstruction (Northeast India-Based Single-Centre Experience). Indian J Surg Oncol. 2019; 10(4):649-653.
- Sukumar V, Ravindran C, Prasad RV. Demographic and Etiological Patterns of Gastric Outlet Obstruction in Kerala, South India. N Am J Med Sci. 2015; 7(9):403-6.
- Maharshi S, Puri AS, Sachdeva S, Kumar A, Dalal A, Gupta M. Aetiological spectrum of benign gastric outlet obstruction in India: new trends. Trop Doct. 2016; 46(4):186-191.
- Khullar SK, DiSario JA. Gastric outlet obstruction. Gastrointest Endosc Clin N Am. 1996 ;6(3):585-603.
- Godadevi TSRSV, Reddy RA. A Clinical Study and Management of Gastric Outlet Obstruction in Adults. Int J Sci Stud 2016;4(6):104-108.
- Singha D, Pawar NM, Mazuder AI, Gopalarathnam S, Kumar N, Deka N. Etiological profile of gastric outlet obstruction and its treatment: a hospital based prospective study in a tertiary care center, north-east India. Int. J. of Adv. Res. 2017; 5 (1). 2258-2264.
- Tendler DA. Malignant gastric outlet obstruction: bridging another divide. Am J Gastroenterol 2002; 97:4.
- Bodh V, Sharma B, Kumar R, Sharma R. Current Trends in Etiological Profile of Acute Upper Gastrointestinal Bleeding in Northern India: A Retrospective Analysis of 5-Year Endoscopic Data. Journal of Digestive Endoscopy 12 (2021): 031 - 035.