48uep6bbphidcol2|ID
48uep6bbphidvals|3058
48uep6bbph|2000F98CTab_Articles|Fulltext
Angiodysplasias also known as vascular ectasias are one of the most common causes of lower intestinal bleeding, particularly in patients older than 60 years and in patients having co-morbidities such as aortic stenosis, chronic renal failure, COPD, cirrhosis. These lesions are most commonly located in caecum and ascending colon, are usually multiple and typically less than 5mm in diameter1. More than 90% of bleedings are minor and resolve spontaneously presumably due to their venous origin, although a few (10%) can present with massive hemorrhage2. We would like to report an interesting case of lower GI bleed in a young 25-year-old female patient in her third trimester of pregnancy and management of such cases.
Case Report
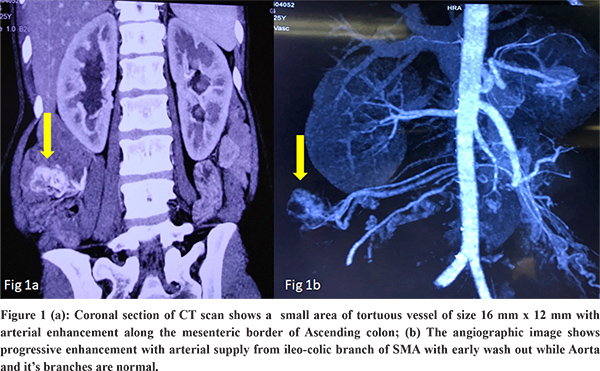
A 25-year-old lady in her 7th month of gestation presented to hospital with complaints of intermittent episodes of bleeding per rectum for the past 6 months along with symptoms of anemia. The bleeding was painless, maroon colored and mixed with stools. Her previous pregnancy was uneventful and had delivered a full-term normal delivery. At admission she had tachycardia (pulse rate 110/ min), BP was 104/74 mm Hg and respiratory rate was 18/min. Her abdomen on examination was soft, non-tender and there was no hepatosplenomegaly or free fluid. Her initial hemoglobin was 6.9g%, total leucocyte count (TLC) 1,2000/mm3, total serum protein 5.6g/dl and serum albumin of 3.0g/dl. She had received 6 units of packed RBC transfusions for intermittent bleeding per rectum over a period of 3 months. She was regularly evaluated with fetal Doppler ultrasound for fetal well-being and was confirmed to carry a single live healthy intrauterine fetus. Esophago-gastro-duodenoscopy was unremarkable while full length colonoscopy including the terminal 10 cm of ileum, revealed presence of altered blood throughout the colon and no blood in the terminal ileum. However, no active bleeding site or any lesion could be identified. Due to anticipated radiation hazard to the mother and fetus CECT Angiography was not contemplated. MRI whole abdomen with MR Angiography was performed, which also failed to show any vascular abnormality or lesion. Meanwhile she was started on tocolytics (uterine relaxants) to delay child birth and dexamethasone to enhance maturity of the fetal lungs by the obstetrician.Since she continued to have intermittent bleeding episodes per rectum with consistent fall in hemoglobin requiring transfusions, CT Angiography of the abdomen was performed in 3rd trimester of pregnancy. It showed small areas of tortuous vessels (16x12 mm) with arterial enhancement and early wash out along the mesenteric border of proximal ascending colon suggestive of angiodysplasia or AV Malformation (Figure 1a). This lesion received supply from ileocolic branches of SMA and drained into the SMV (Figure 1b).
Despite conservative medical management for 4 weeks, intermittent bleeding requiring regular blood transfusions continued unabated. After a detailed counselling about the nature of disease and treatment options available and taking due risk consent to the mother and fetus, patient was taken up for Open Right Hemicolectomy in the presence of obstetrician (Figure 2). The histopathology revealed flattened mucosa with multiple dilated and tortuous blood vessels spurting through mucosa suggestive of angiodysplasia. Remaining crypt architecture was normal. The post-operative period was uneventful. The patient was allowed oral intake from POD-2 and was discharged on POD-5. Patient developed surgical site infection (SSI)grade -3, which was managed by regular dressings. The patient went on to continue pregnancy for another 2 weeks and had a normal vaginal delivery at full-term. The mother and child were doing well at 1 year follow up.
Discussion
The prevalence of colonic angiodysplasia (AD) has been reported to be approximately 1%3. It is the most common vascular malformation of the GI tract in the general population. They may be asymptomatic or may present with GI bleed. Bleed in a majority of these patients is mild, recurrent and chronic and well compensated while some of them may present with acute life-threatening bleeding. 51-89% of angiodysplasias of the GI tract are found in the caecum and ascending colon. 3-40% of colonic angiodysplasias are responsible for lower gastrointestinal bleed in various series. These lesions are synchronous in about 20% of patients. Our patient was a young 25-year-old expectant mother who presented with recurrent episodes of lower intestinal bleeding requiring transfusions. Such a presentation is unusual and rare in patients of angiodysplasia of colon. It was a single lesion of size 16x12 mm on angiography and after resection, the lesion was measured to be 30 mm in diameter. She had no comorbidities like chronic renal disease to account for her rare presentation, which is a well-known cause for early presentation in patients of angiodysplasia. Her presentation in the last trimester of pregnancy was unique and made the management of this lesion challenging. It is the first case of this kind to be reported in the literature to our knowledge. We assume that the hormonal effects of progesterone and oestrogen during pregnancy has a role in the formation of new vascular lesions like angiodysplasia and this has not been reported in literature. The etiology and mechanism of development of angiodysplasia is not fully known and needs further study.
Endoscopy is currently the main tool for diagnosing angiodysplasia which shows a ‘Pale halo’ sign. In our index case Colonoscopy couldn’t locate the exact site of lesion as altered blood was seen throughout the colon, making any kind of intervention difficult. Other investigations useful in localising bleeding include, radionuclide scanning, Tc99m RBC scan, conventional angiography, CT or MR angiography. Standard Angiography although allows accurate localisation and therapeutic embolizationin the same sitting, but carries a small risk of bowel ischemia. In our case we re-evaluated the patient with CT angiography after failing to localize the bleed using MR angiography. Presentation in the third trimester of pregnancy limited our options of evaluating the lesion with imaging and the potential management options.
Various treatment modalities are available for treatment of symptomatic colonic angiodysplasia. Argon plasma coagulation - This is the most widely used method to treat angiodysplasia. Electrocoagulation, Photocoagulation -ND: YAG and Argon lasers are also used with no serious complications. Endoscopic clips are also useful. Transcatheter angiography and intervention - These are used instead of surgery in high-risk patients, for inaccessible lesions or to localise the lesion prior to surgery. Hormonal therapy-Previous studies utilized high doses of ethinyl oestradiol (up to 0.05 mg) to effect a treatment response in angiodysplasia. However, a recent RCT showed that regular oestrogen-progesterone treatment is not useful in the prevention of re-bleed from gastrointestinal angiodysplasia4.
Surgical resection is reserved for patients with acute severe bleeding not controlled by other means, patients with recurrent chronic bleeding who are transfusion dependent. It is also used for patients in whom the source of blood loss is clearly identified but none the less other treatment options to control the ongoing bleed have failed. There is no evidence in literature about the prevalence and management of symptomatic colonic angiodysplasia during the third trimester of pregnancy. The safe outcome of the mother and fetus was accomplished by prolonging the pregnancy with tocolytics, hastening fetal lung maturation, safe anaesthesia and surgical resection of the bleeding colonic lesion.
Colonic angiodysplasias may be asymptomatic or may present with life threatening lower GI bleed. This is the first reported case of a safe Right Hemicolectomy done on a pregnant patient in her third trimester with symptomatic ascending colon angiodysplasia.
References
- Danesh BJ, Spiliadis C, Williams CB, ZambartasCM.Angiodysplasia-an uncommon cause of colonic bleeding: colonoscopic evaluation of 1,050 patients with rectal bleeding and anaemia.Int J Colorectal Dis. 1987;2:218
- Cappell MS, Gupta A.Changing epidemiology of gastrointestinal angiodysplasia with increasing recognition of clinically milder cases: angiodysplasia tend to produce mild chronic gastrointestinal bleeding in a study of 47 consecutive patients admitted from 1980-1989.Am J Gastroenterol. 1992;87:201.
- S. Ueno, H. Nakase, K. Kasahara et al, “Clinical features of Japanese patients with colonic angiodysplasia,” J Gastroenterol Hepatol, 23 (2008), pp. e363-e366.
- Junquera F, Feu F, Papo M, et al. A multicenter, randomized, clinical trial of hormonal therapy in the prevention of rebleeding from gastrointestinalangiodysplasia. Gastroenterology. 2001;121(5):1073-1079.