48uep6bbphidcol2|ID
48uep6bbphidvals|3057
48uep6bbph|2000F98CTab_Articles|Fulltext
Situs ambiguous, also known as heterotaxy syndrome, is defined as abnormal positioning of organs and vessels in thorax and abdomen which results from errors in left-right patterning during embryogenesis1. Incidence of situs ambiguous is approximately 1 in 40,000 live births with male: female ratio of 2:12. Situs ambiguous has been described mainly in paediatric age group. There is limited literature available on manifestations of situs ambiguous in adults. Congenital heart disease is present in 90-99% of these patients, more in asplenia group. Incidence of patients with polysplenia surviving into adulthood is only 5%2. Laparoscopic cholecystectomy in heterotaxy syndrome is a unique challenge for operating surgeons because of abnormal position of gall bladder and liver with altered anatomy of structures in hepatoduodenal ligament (HDL). Herein we report a case of successful laparoscopic cholecystectomy in a 50-year-old male patient with heterotaxy syndrome with polysplenia who presented with gall bladder (GB) perforation with subhepatic collection and historyof open partial cholecystectomy elsewhere.
Case Report
A 50-year-old male patient presented to our hospital with history of intermittent pain right upper abdomen requiring intravenous (IV) analgesics with on and off episodes of fever for 1 month. He had a history of getting surgery elsewhere for symptomatic gall stone disease 6 years back for which open partial cholecystectomy was done because of dense adhesions and abnormal anatomy. He was a diagnosed case of complete heart block for which cardiac pacemaker was inserted 10 years back. He was a known case of diabetes mellitus on oral hypoglycemic agents. On per-abdomen examination there was presence of healed right subcostal scar and tenderness in right hypochondriac and epigastric region with enlarged left lobe of liver. His total leucocyte count (TLC) was 14,000 with 92% polymorphs with normal liver function test (LFT).
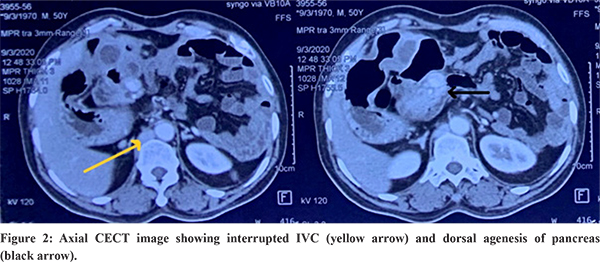
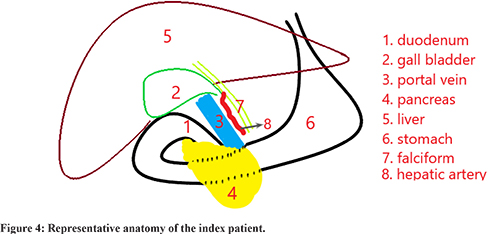
On ultrasonography(USG), 5x3 cm tubular cystic folded lesion was seen in GB fossa placed medially with multiple wall calcification and multiple echogenic calculi within and abnormal common bile duct (CBD), hepatic artery and portal vein relationship with subhepatic collection. He was further evaluated with contrast enhanced computed tomography (CECT) of abdomen which showed thick walled loculated collection in GB fossa measuring approximately 5x4.5x3.3 cm with mild surrounding inflammatory changes suggestive of sealed GB perforation. Other findings were multiple splenunculi, enlarged liver, Preduodenal portal vein, dorsal agenesis of pancreas and interrupted infrahepaticsuprarenal inferior vena cava (IVC) with presence of posthepatic segment of IVC [Figure 1 & 2]. USG guided aspiration of collection was done and patient was managed with IV antibiotics based on pus culture and sensitivity. Patient improved symptomatically. Four weeks later patient was planned for elective cholecystectomy. Magnetic retrograde cholangiopancreatography (MRCP) was planned to have a roadmap in view of abnormal HDL anatomy, but could not be done because of presence of cardiac pacemaker. CECT was reviewed on console and patient was later taken up for surgery. CECT abdomen revealed posterior relationship of CBD to common hepatic artery (CHA) and portal vein (PV). Cystic duct was placed between CHA and PV.

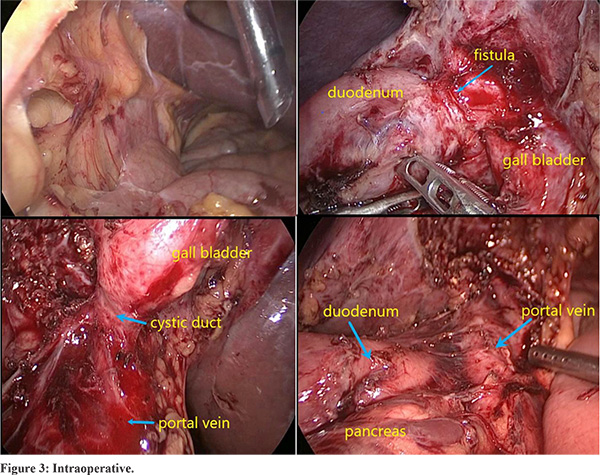
Cardiac pacemaker setting was changed prior to surgery. Laparoscopic cholecystectomy was performed under general anaesthesia 4 weeks after aspiration. First 11 mm camera port was inserted in supraumbilical region by open technique. Other 5 mm and 12 mm ports were placed in left lumbar and left subcostal region in mid clavicular line, respectively. After adhesiolysis, 5 mm port was placed in right hypochondrium in anterior axillary line. Intraoperatively, GB was found in midline. Dense adhesion was present between GB and duodenum with suspicious communication. Gall bladder was separated from duodenum and duodenum was repaired. PV was placed anteriorly [Figure 3]. Antegrade cholecystectomy done. Cystic duct was delineated and divided using stapler.
Total duration of surgery was 120 minutes and intraoperative blood loss was 100 ml. Drain was removed on POD 2 and patient was discharged on POD 3. GB histopathology report was suggestive of chronic calculous cholecystitis with antral metaplasia. The patient is doing well in the follow up.
Discussion
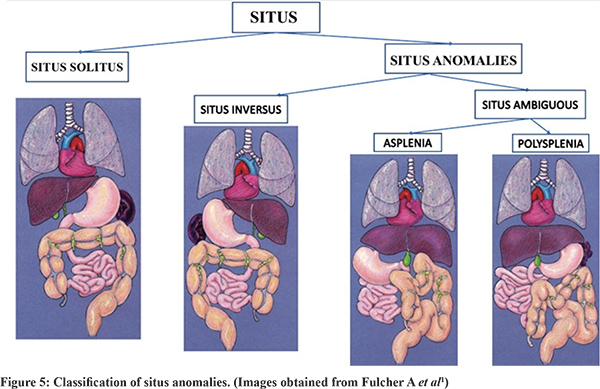
Situs ambiguous, also known as heterotaxy syndrome, is disordered arrangement of organs and vessels in thorax and abdomen. It differs from orderly arrangement of truncal organs in either the typical anatomy (situs solitus) or the mirror image of it (situs inversus)1. Situs ambiguous has been classified into two major groups described by Fulcher et al: with polysplenia, also called polysplenia syndrome and left isomerism (patients only have two bilateral lung lobes), and with asplenia, also called asplenia syndrome or right isomerism (patients only have three bilateral lung lobes)1 [Figure 5]. Situs ambiguous is a rare entity with incidence of approximately 1 in 40,000 live births with male: female ratio of 2:12. Asians show a higher prevalence of heterotaxy syndrome compared to western population. No single etiological factor is responsible for heterotaxy as concluded in various studies3.
Constellation of cardiac findings in subgroup of patients with heterotaxy syndrome differ in two groups. Patients with asplenia have total anomalous pulmonary venous connection, unbalanced atrioventricular septal defect, double outlet right ventricle, pulmonary atresia, absent coronary sinus and bilateral “right atrial like” appendages. Patients with polysplenia have less severe cardiac defects, IVC interruption with azygos or hemiazygos continuation, atrioventricular septal defect (with balanced ventricles) and bilateral “left atrial like” appendages4. This syndrome with left isomerism has strong association with sinus node dysfunction or congenital heart block5. Our patient had IVC interruption and complete heart block with cardiac pacemaker in situ. Complex cardiac anomalies are the most common cause of mortality in paediatric age group. In patients with asplenia congenital heart disease (CHD) occurs in 99-100% of cases.
Most of the adult patients with situs ambiguous are asymptomatic. Therefore, heterotaxy polysplenia syndromes are often detected incidentally by CECT abdomen or magnetic resonance imaging (MRI) for evaluation of other medical diseases. Multiple splenules of various size are characteristically found in polysplenia located always adjacent to stomach because of common embryonal development within mesogastrium as reported in this patient6 [Figure 1]. Other findings in polysplenia syndrome are dorsal pancreatic agenesis, annular pancreas, malrotation or nonrotation of gut7.
Most frequent hepatobiliary abnormalities are positional abnormalities, presence of midline liver and GB, very prominent left lobe of liver as seen in our patient8. Preduodenal portal vein (PDPV) is rare anomaly found in polysplenia syndrome. PDPV is associated with biliary tract obstruction, long standing malnutrition, selective portal vein obstruction and cholelithiasis9. Presence of PDPV can cause technical difficulties during laparoscopic cholecystectomies and can increase complications like haemorrhage. Our patient had PDPV hence the HDL area had been handled very carefully [Figure 3].
Abdominal imaging like USG, CECT abdomen and MRCP provide a roadmap to abdominal surgeries particularly hepatobiliary surgeries because of altered anatomy of HDL structures. In our patient USG and CECT revealed abnormal relationship between CBD, PV and hepatic artery. MRCP could not be done because of presence of cardiac pacemaker that added to more difficulty. Laparoscopic cholecystectomy in our case was technically more challenging due to presence of dense adhesions due to previous surgery and history of GB perforation. Though more challenging, laparoscopic cholecystectomy could be performed successfully in our patient with uneventful postoperative course.
In conclusion, laparoscopic cholecystectomy is safe and feasible in heterotaxy polysplenia syndrome, although technically more challenging. Abnormal relationship between cystic duct, CBD, PV and CHA should be kept in mind and should be preoperatively evaluated.
References
- Fulcher AS, Turner MA. Abdominal Manifestations of Situs Anomalies in Adults. Radiographics. 2002; 22:1439- 56.
- Ware SM, Peng J, Zhu L, Fernbach S, Colicos S et al. Identification and Functional Analysis of ZIC3 Mutations in Heterotaxy and Related Congenital Heart Defects. Am. J. Hum. Genet. 2004; 74:93-105.
- Kim SJ. Heterotaxy syndrome. Korean Circulation Journal. 2011;41:227-32.
- Uemura H, Ho SY, Devine WA, Anderson RH. Analysis of visceral heterotaxy according to splenic status, appendage morphology, or both. Am J Cardiol. 1995;76:846–9.
- Wolla CD, Hlavacek AM, Schoepf UJ, Bucher AM, Chowdhury S. J. Cardiovascular manifestations of heterotaxy and related situs abnormalities assessed with CT angiography. Cardiovasc Comput Tomogr. 2013;7:408-16.
- Muneta S, Sakai S, Fukuda H, Imamura Y, Matsumoto I. Polysplenia syndrome with various visceral anomalies in an adult: embryological and clinical considerations. Intern Med. 1992;31:1026-31.
- Maier M, Wiesner W, Mengiardi B.Annular pancreas and agenesis of the dorsal pancreas in a patient with polysplenia syndrome. Am J Roentgenol. 2007;188:150-3.
- Gagner M, Munson JL, Scholz FJ.Hepatobiliary anomalies associated with polysplenia syndrome. Gastrointest Radiol. 1991;16:167-71.
- Seo HI, Jeon TY, Sim MS, Kim S. Polysplenia syndrome with preduodenal portal vein detected in adults. World J Gastroenterol. 2008;14:6418-20.