48uep6bbphidcol2|ID
48uep6bbphidvals|3053
48uep6bbph|2000F98CTab_Articles|Fulltext
Stent fracture is one of the rare causes of trans-jugular intrahepatic portosystemic shunt (TIPS) dysfunction and is identified as a risk factor for stent thrombosis. Various factors such as long segment stents, multiple overlap stents, stent across bends, and mechanical stress account for stent fracture.1 Awareness of this complication is very important to identify and manage early trans-jugular intrahepatic portosystemic shunt (TIPS) dysfunction. We report a case of stent fracture presented with TIPS shunt dysfunction and managed successfully by stent revision.
Case Report
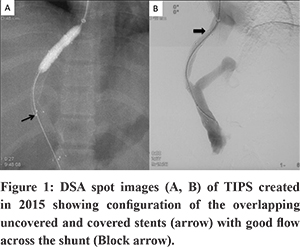
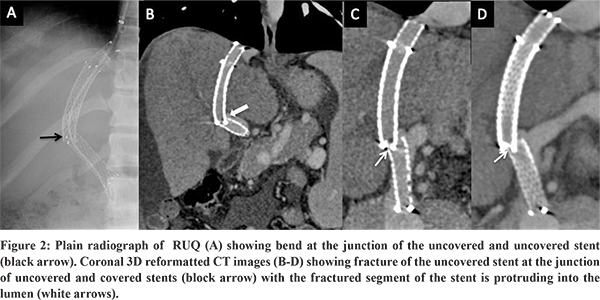
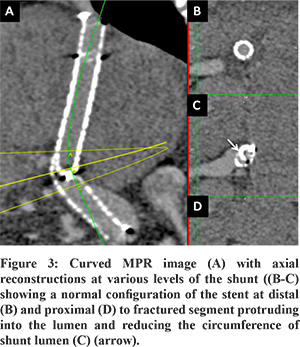
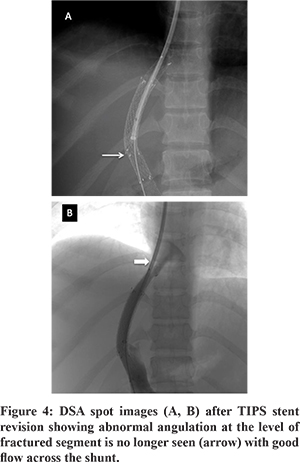
A 27-year-old female presented with abdominal distention and loss of appetite for 2-months. She was a known case of hepatic venous outflow tract obstruction for which she had undergone TIPS five years back. (Figure 1) She was on regular anticoagulation. Doppler of the TIPS stent showed some angulation at the junction of covered and uncovered stent near the portal end of the stent, but the flow in the stent was preserved. The patient had moderate ascites as well. The patient was advised liver function tests as a part of the workup to evaluate ascites.Liver function tests were normal. A CT portography was done to look for any abnormality in the TIPS stent. CT portography revealed a normal flow of contrast through the stent. However, there was acute angulation noted at the junction of covered (Fluency Plus, Angiomed GmbH/C. R. Bard, Inc., Karlsruhe, Germany) and uncovered stents (E-Luminexx Vascular Stent, Bard Peripheral Vascular, Tempe, Arizona) with the fracture noted in the uncovered stent with the fractured segment of stent protruding into the lumen and reducing the circumference of shunt lumen (Figure 2, Figure 3). TIPS revision was planned, because of persistent ascites, to correct abnormal stent morphology due to fracture of the uncovered stent.Diagnostic angiogram of TIPS stent revealed flow across the shunt without any thrombosis. A 10 mm x 10 cm covered stent (Fluency Plus, Angiomed GmbH/C. R. Bard, Inc., Karlsruhe, Germany) was placed centered at the site of fracture. Post covered stent placement, there was a correction of the abnormal angulation of the TIPS stent and the fractured stent was no longer causing any luminal impingement. (Figure 4) There was complete resolution of ascites at one month follow-up, and Doppler showed normal flow (>100cm/sec) across the TIPS stent.
Discussion
Stent fractures are common in arterial circulation but rare in venous circulation1. Stent fracture may occur late as a result of mechanical fatigue or early in association with suboptimal deployment. There are various risk factors or theories that have been ascribed to causes of stent fracture, such as long segment stents, multiple overlap stents, stent across bends or joints, and a variety of mechanical stress leading to fatigue failure of nitinol stent. Incidence of stent fracture has been reported in a wide range of 2%-65% in the superficial artery.1 Three cases of TIPS stent fracture have been reported in the literature, to our knowledge. (Table 1) Zabicki et al. reported a case of stent fracture in a case of cirrhosis with refractory variceal bleed.2 The fracture was caused due to abnormal angulation of the TIPS stent leading to high bending stress. The site of fracture was the bare metal stent at the hepatic venous end, with the fractured fragments of stent lying in the IVC and right atrium. The flow through the TIPS stent was maintained, the patient remainedasymptomatic and managed conservatively. Ding et al. reported a case of TIPS stent fracture in a cirrhotic patient.3 The fracture involved the uncovered stent at the hepatic venous end with a displacement of the fractured fragment into the right atrium. As proposed by the authors, the fracture mechanism was stress at the junction of the covered and uncovered stent due to respiratory motion at the hepatic venous end. The patient was asymptomatic with a patent TIPS stent and treated conservatively. Komaki et al. reported another case in which was the site of fracture was at the junction of the covered and uncovered stent at the hepatic venous end of the stent.4 In our case, the fracture site was also at the junction of the covered and uncovered stent but at the portal venous end of the stent.In our case, the covered stent extended up to the hepatic venous opening in the IVC. The likely mechanism was due to high bending stress at the junction of the covered and uncovered stent due to slight angulation in the TIPS stent. There was no displacement of the fractured stent fragment. However, the fractured fragment was protruding into the lumen shunt. In our case, the patient presented with ascites due to partial impedance to the flow across the stent. All three cases of TIPS stent fracture previously reported in literature occurred at the hepatic venous end and the stent did not extend up to the hepatic vein ostia; as a result, there was potential bending stress at the junction of the covered and uncovered stent, which was aggravated by the increased respiratory motion near the hepatic venous end of the stent. In our case, the covered stent extended up to the hepatic vein ostia, thusthe junction of the covered and uncovered at the portal venous end was the vulnerable point.
TIPS stent fracture is very rare and the presence of TIPS stent angulation and use of overlapping covered and uncovered stents increases the risk of stent fracture with the most common site being the junction of covered and uncovered stents. The use of a single piece stent like the VIATORR stent-graft (Gore, Flagstaff, AR, USA) is thus ideal to decrease the risk of stent fracture rather than using two overlapping stents. Our case is unique compared to the other case reports because it represents the first case of TIPS stent fracture at the portal venous end of the stent with no displacement of the fractured fragment. Our patient was symptomatic and responded to stent revision with a covered stent graft across the fractured segment.
References
- Tielliu IFJ, Zeebregts CJ, Vourliotakis G, Bekkema F, van den Dungen JJAM, Prins TR, et al. Stent fractures in the Hemobahn/Viabahn stent-graft after endovascular popliteal aneurysm repair.J Vasc Surg. 2010 Jun;51(6):1413–8.
- Zabicki B, Ricke J, Dudeck O, Pech M. CT-assisted transfemoral intrahepatic portosystemic shunt in a long duration follow-up: A case report.Pol J Radiol.2014 Feb 27;79:39–41.
- Ding P-X, Han X-W, Hua Z-H, Liu C. Stent Fracture and Fragment Migration to Chordae Tendineae of the Tricuspid Valve after Transjugular Intrahepatic Portosystemic Shunt Procedure. J VascIntervRadiol JVIR. 2017;28(9):1293–5.
- Komaki T, Hiraki T, Uka M, Fujiwara H, Iguchi T, Kanazawa S. A Case of Stent Fracture After Transjugular Intrahepatic Portosystemic Shunt. Cardiovasc InterventRadiol. 2018 Jun 1;41(6):976–8.