48uep6bbphidcol2|ID
48uep6bbphidvals|3042
48uep6bbph|2000F98CTab_Articles|Fulltext
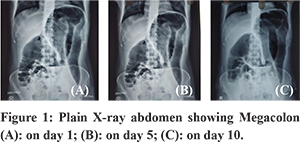
Toxic megacolon is a severe complication of Clostridium difficile infection (CDI) and is seen in about 8% of pseudomembranous colitis patients. The clinical manifestations of toxic megacolon are shock and severe ileus with or without diarrhoea. However, patients with no prior illness and no antibiotic exposure rarely present with toxic megacolon with community-acquired CDI. We present a case of toxic megacolon who had no exposure to antibiotics in the last six months without any comorbidities. Further, this community-acquired CDI with dilated colon persisted for almost ten days and was managed successfully with medical management using 5- Hydroxy-tryptamine receptor 4 (5HT4) agonist.
Case Report
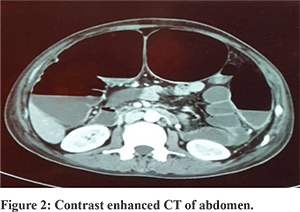
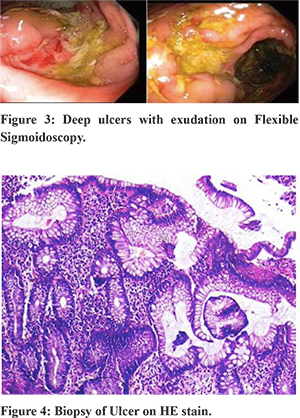
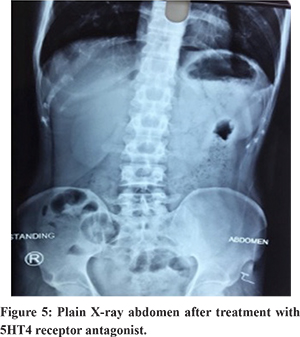
A 38-year-old male, without any comorbidities presented with complaints of abdominal pain and distention of 8 days duration without any history of vomiting, diarrhoea, blood in stools, or weight loss. There was no history of any prior antibiotic exposure in the last six months. On admission, his temperature was 101.40F, and pulse rate was 110/min regular. His abdomen was distended with a tympanic note without any evidence of free fluid. Bowel sounds were sluggish. His hemogram showed Hb of 8.6g/dl, total WBC count of 18400 with 85% polymorphs and 10% lymphocytes platelet count of 4.5 lakhs/dl. Stool analysis showed multiple WBCs and RBCs. Erect skiagram of the abdomen showed a massively dilated colon with a maximum diameter of 7.3 cm (Figure 1-A). Contrast-enhanced CT of the abdomen revealed massively dilated transverse colon (7-7.5 cm) and ascending colon (6.5 cm) with loss of haustral markings (Figure 2). He was started with conservative management. In the next 24-48 hours, his pain in abdomen decreased; however, abdomen continued to remain bloated with a tympanic note. There was no decrease in the size of dilated loops of the colon on plain skiagram of the abdomen. There was mild diffuse tenderness but no rebound tenderness. Seeing no change in dilated colonic diameter with definite clinical improvement, conservative management was continued with endoscopic decompression. Sigmoidoscopy showed multiple large deep irregular ulcers with whitish exudates at the junction of the sigmoid and descending colon (Figure 3). However, there was no change in the colon’s diameter after decompression. The biopsy from ulcers showed ulcerated mucosa with neutrophilic infiltration, and moderate lymphoplasmacytic infiltrate in lamina propria, without any granuloma, malignancy (Figure 4). Further investigations with AFB staining on biopsy, TB PCR, CMV PCR were negative. Stool for C. diff. toxin was positive, and he was started on vancomycin and metronidazole. His clinical condition improved further with no change in colonic dilatation even on day five (Figure 1-B) but because of significant clinical improvement, he was started with clear liquids. He started eating soft semisolid food with bowel movement, but there was no decrease in the diameter of colonic loops even after ten days of conservative management (Figure 1-C). The second sigmoidoscopy at this stage showed deep circumferential ulcer at the same site without any exudation. Biopsy revealed extensive ulceration with granulation tissue, occasional crypt abscesses with focal muco-depletion and crypt branching. Even after the second endoscopic decompression, there was no change in the diameter of the colon. At this stage, the patient was started with prucalopride which further improved his clinical condition with normalization of the dilated colon (Figure 5). At six months, follow up patient is asymptomatic.
Discussion
This is a rare case of CDI induced toxic megacolon which persisted almost for ten days despite aggressive medical therapy. Endoscopic decompression has been tried successfully in the past to treat persisted megacolon, but in this case, it was tried twice without any success. It is possibly because of the penetration of toxin into muscularis mucosa, which leads to persistent megacolon for almost ten days despite clinical improvement. The probable mechanism of prolonged ileus is toxin B induced spontaneous and carbachol-induced intestinal smooth muscle contractions4. It is probably mediated by increased synthesis of NO due to upregulation of production of inducible nitric oxide synthase, which in turn increases nitric oxide, and thus causes dilation of the colon. Because of persistent megacolon 5-HT4 agonist, Prucalopride was given to improve the colonic motility. Prucalopride is a highly selective serotonin 5-HT4 receptor agonist which has been shown to stimulate gut motility in vitro and vivo5. In this case use of prucalopride increased the colonic motility thereby resulting in improvement in symptoms and colonic diameter.
This case highlights two important messages; firstly CDI presenting as toxic megacolon which is an uncommon presentation that too in a patient who has not been exposed to antibiotics suggesting the increasing prevalence of community-acquired C difficile infection.Secondly, it emphasizes the possible role of 5-HT4 agonist on toxic megacolon and opens the idea of using 5-HT4 agonist in megacolon of other aetiology and intestinal pseudo-obstruction.
References
- Elinav E, Planer D, Gatt ME.Prolonged ileus as a sole manifestation of pseudomembranous enterocolitis. Int J Colorectal Dis 2004;19:273–276.
- Rybolt AH, Bennett RG, Laughon BE, etal., Protein-losing enteropathy associated with Clostridium difficile infection. Lancet. 1989;17:1353-5.
- Ikuhara M, Tsang TK, Tosiou A, White EM, etal., Intussusception in an adult with pseudomembranous colitis. J Clin Gastroenterol. 1995;21:336-8.
- Gilbert RJ, Pothoulakis C, LaMont JT. Effect of purified Clostridium difficile toxins on intestinal smooth muscle. II. Toxin B. Am J Physiol.1989;256(4 Pt 1):G767-72.
- Sanger GJ, Quigley EM. Constipation, IBS and the 5-HT4 receptor: What role for prucalopride? In Clinical Medicine Insights: Gastroenterology.2010;3:21-33.