48uep6bbphidcol2|ID
48uep6bbphidvals|3008
48uep6bbph|2000F98CTab_Articles|Fulltext
Rectal prolapse is a debilitating condition, commonly seen in elderly females. However, it may be seen at any age and in both genders. Protrusion of the rectum out of the anus during defecation is the commonest symptom. Most of the time, it reduces on its own or patients can reduce it manually. Pain, bleeding per rectum, mucus discharge, constipation and faecal incontinence are the other symptoms. Rarely, a prolapsed rectum may fail to reduce. Irreducibility leads to vascular compromise, obstruction and gangrene of the prolapsed rectum and requires emergent surgical intervention. There are more than 100 different surgical interventions described for rectal prolapse. These procedures are done by abdominal, perineal or by sacral approaches. The goal of surgical intervention in an elective setting is to avoid recurrence with low morbidity.
Irreducible rectal prolapse is a rare entity and the best procedure to deal with this emergency is not well elucidated1. In an emergency condition, protecting the life of the patient becomes the primary goal of any surgical intervention. Considering life salvage as the primary goal, a straight forward procedure to overcome the emergency is preferred. However, the best procedure to deal with such a scenario may not be easy to choose, especially when it is associated with a congenital anomaly. We describe here a case of irreducible rectal prolapse in a patient with an anorectal malformation and the management pathway we followed in the case.
Case Report
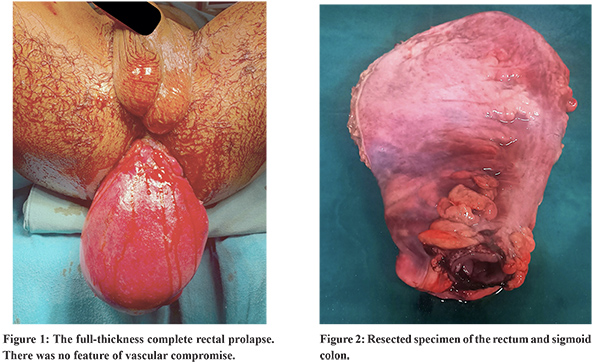
Our patient was a 35-year-old male from Haryana, India. He was admitted to the Emergency Department with complaints of mass descending peranum. The mass used to come out during defecation since childhood and he had learnt to reduce it manually by pressing it with his fingers. For the last two days, he was unable to reduce it. He had faecal incontinence with a Wexner score of 12/20. The patient was born with an anorectal malformation. A diversion colostomy was made 2 days after birth. Surgical reconstruction of the anus was done at 12 months of age and colostomy was reversed after 1 month of reconstruction of the anus. On evaluation, he had complete rectal prolapse without any features of vascular compromise (Figure 1). Attempts to reduce it manually failed. He was taken for manual reduction of the prolapse with anal encirclement (Thiersch procedure) under laryngeal mask anaesthesia. However, the prolapse could not be reduced. He was subsequently put on general anaesthesia with endotracheal intubation with consent for possible resection and stoma. A laparotomy was performed and an attempt was made to reduce the prolapsed rectum by external pressure from the perineum and internal traction from within the pelvis. However, this attempt of internal reduction also failed. Finally, a perineal proctosigmoidectomy (Altemeier’s procedure) was performed. The rectal wall was incised across its full thickness and sectioned just above the dentate line. The prolapsed rectum and sigmoid colon were resected (Figure 2) and a manual coloanal anastomosis was made.A diversion colostomy was done. The patient made an uneventful recovery and was discharged on the sixth postoperative day. At two months of follow up, he is doing fine and waiting for reversal of the stoma.
Discussion
This case highlights the need to be cognizant of various techniques available for a surgical condition. Rectal prolapse in itself is not a common disease. So, the availability of expertise may be scarce and more so in an emergent situation. In our routine practice, the preferred procedures for rectal prolapse are either laparoscopic repair with prosthetic mesh or a Delorme procedure. In the present case initially, our plan was manual reduction of the prolapse with anal encirclement (Thiersch procedure) under short general anaesthesia. Simple reduction with anal encirclement is known to be associated with high recurrence. However, in view of the ongoing COVID-19 pandemic, we planned a less invasive procedure and tried to avoid endotracheal intubation. Also, the simple reduction would bridge the emergent situation and a definitive procedure could be planned electively. A few other anecdotal conservative methods like direct application of granulated table sugar, hyaluronidase or elastic compression wrap are also described to reduce oedema and facilitate reduction2.
In our case, as the prolapse was not reduced after laparotomy and bimanual manoeuvre, a perineal proctosigmoidectomy was required as a salvage procedure. Perineal proctosigmoidectomy (Altemeier procedure) is an established procedure for rectal prolapse. It is associated with a recurrence rate ranging from 0-10%3. However, the procedure is inherently associated with a low colorectal anastomosis. Any leak from such anastomosiscan lead to significant morbidity and mortality. Hence, the Altemeier procedure, although associated with low recurrence, is not a preferred technique for many. We adopted the Altemeier procedure as the last resort when all other attempts failed. In a situation like long-standing irreducible prolapse with vascular compromise, an Altemeier procedure would have been the first option4. We added a diversion colostomy as the rectum was edematous due to irreducible prolapse and the patient had a surgically constructed anus with an unknown vascular supply of the distal segment.
Another interesting aspect was that our patient had an anorectal malformation at birth, and the anus was surgically reconstructed. A surgically reconstructed anorectum or a patient with an anorectal malformation (ARM), may be inherently associated with increased risk of rectal prolapse. In patients requiring colostomy at birth, as in our case, the rectum is subjected to increased peristaltic force once the colostomy is reversed after definitive repair. The quality of perineal muscles and improper surgical techniques are other factors responsible for the appearance of prolapse after ARM surgery5.
Conclusion
We report a complication of rectal prolapse in a patient with a surgically constructed anus.Altemeier procedure may be the saviour in such a situation.
References
- van der Schans EM, Paulides TJC, Wijffels NA, Consten ECJ. Management of patients with rectal prolapse: the 2017 Dutch guidelines. Tech Coloproctology. 2018;22(8):589–96.
- Sarpel U, Jacob BP, Steinhagen RM: Reduction of a Large Incarcerated Rectal Prolapse By Use of an Elastic Compression Wrap. Dis Colon Rectum, 2005; 48: 1320–22
- Ris F, Colin J-F, Chilcott M, Remue C, Jamart J, Kartheuser A. Altemeier’s procedure for rectal prolapse: analysis of long-term outcome in 60 patients. Colorectal Dis. 2012;14(9):1106–11.
- Cernuda RB, Ángel JP, Fernández NT, Sánchez-Farpón JH, Pérez JAÁ. Perineal Rectosigmoidectomy (Altemeier Procedure) as Treatment of Strangulated Rectal Prolapse. J Gastrointest Surg. 2016;20(12):2102–3.
- Brisighelli G, Di Cesare A, Morandi A, Paraboschi I, Canazza L, Consonni D, et al. Classification and management of rectal prolapse after anorectoplasty for anorectal malformations. Pediatr Surg Int. 2014;30(8):783–9.