48uep6bbphidcol2|ID
48uep6bbphidvals|2993
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Kidney is most commonly involved organ in amyloidosis. Liver is involved in 10% cases of amyloidosis.1 Most of the these patients present with abdominal enlargement that can be due to hepatomegaly with or without splenomegaly or ascites. Few patients also present with jaundice which at times can be very severe or esophageal varices as a manifestation of portal hypertension.2 Rapid enlargement in size of liver can lead to abdominal pain & rarely patient may present with spontaneous hepatic rupture.3 The gold standard for the diagnosis of hepatic amyloidosis is demonstration of apple green birefringence with Congo red staining on paraffin embedded tissue sections.4 Liver can be involved in primary (AL) or secondary amyloidosis. Other organs like kidney, gastrointestinal tract & spleen etc. can also be involved. Whenever there is isolated liver involvement, it is known as primary hepatic amyloidosis. Most of the patients with massive hepatic involvement have poor prognosis & usually die within year of diagnosis.5 This study presents a retrospective analysis of clinical presentation.
Materials and Methods
The patients with liver biopsy diagnosis of hepatic amyloidosis from the 2009 to 2016 were selected for the retrospective analytical study. The clinical information and data regarding various routine and special laboratory tests like hemoglobin, blood counts, and liver and renal function tests was obtained from the medical records. Total 26 liver biopsies diagnosed as hepatic amyloidosis were selected for study. Of these three were post-mortem biopsies. Out of remaining 23 cases six biopsies were transjugular liver biopsies (TJLB). Haematoxylin and Eosin stained sections of all the liver biopsies were reviewed. The Masson Trichrome and Congo red staining was done on the all the biopsies. The polarized microscopy was used to demonstrate apple green birefringence of the amyloid. SAA (Serum Amyloid Associated) protein, kappa and lamda immunostains were performed wherever possible.
Results
Most of the patients were adults with median age of 58 years. There was one young boy of 15 years who was a known case of chronic renal failure on maintenance hemodialysis. He was incidentally detected positive for hepatitis B surface antigen so was referred to our centre for further management. Liver biopsy was done to assess the activity of disease. But biopsy showed deposition of amyloid material in the hepatic arterioles. There was male preponderance with Male to female ratio of 10:3(20 males, 6 females).
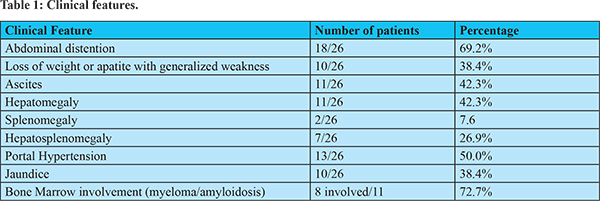
Eighteen out of 26 patients had abdominal distention either due to ascites (n=11), hepatomegaly (n=11), splenomegaly (n=2) or combined hepatosplenomrgaly (n=5). Patients with palpable liver and size more than 15.5 cm on imaging were considered to have hepatomegaly. Similarly patients with palpable spleen and size of 12 cm or more on imaging were considered to have splenomegaly.6-8 Few patients had overlap of the clinical features. Thirteen patients had portal hypertension; all had abdominal distension due to organomegaly or ascites. Two patients with abdominal distension were not having either organomegaly or ascites. (Table 1) One of them was a 61 year old female who presented in with abdominal pain and distension, retrosternal chocking and vomiting. She was known case of intestinal pseudo-obstruction. Her electrocardiogram showed left bundle branch block. Her rectal biopsy was negative for amyloid. Soon after admission she developed cardiac arrest and died in a course of hospital. Post mortem liver biopsy was done which showed sinusoidal amyloid deposits. Hence the diagnosis of cardiac arrest due involvement of conduction system of heart by amyloidosis was done.
Hepatic venous pressure gradient (HVPG) measurement was done in 12 patients. The HVPG readings were ranging from 5-28 mm of Hg. Two patients had HVPG of 5 mm of Hg. Rest of all ten patients had portal hypertension with readings ranging from 7-28 mm of Hg. They were having either varices or various other manifestations of portal hypertension. One post transplant patient had HVPG of 20 mm of Hg but no other manifestation of portal hypertension. This patient had two ante mortem biopsies which showed evidence of rejection and globular amyloid deposits. He had a detrimental clinical course and died within year. His postmortem liver biopsy showed changes related to sepsis like canalicular and ductular cholestasis along with mixed portal inflammation and amyloidosis. Ongoing rejection with sepsis must have had some effect on the hemodyanamics of the liver which might have caused the persistently elevated HVPG but no other manifestation of portal hypertension.9,10 Of the two patients with HVPG reading 5 mm Hg, one had vascular amyloid showing deposits in hepatic arterioles positive for SAA. The other case showed sinusoidal, stromal and vascular deposits but showed hepatomegaly and ascites but no varices.
Transient elastography or fibroscan was done in the five patients. All of them showed median reading of 75kPa. The abdominal imaging records were available in sixteen patients. The craniocaudal liver span in midclavicular line more than 15.5 cm and spleen size more than 12 cm along the longitudinal axis were considered as indicators of Hepatomegaly and splenomegaly.6-8 Seven patients had hepatomegaly on imaging with size ranging from 17 cm to 29.4 cm. Six patients had splenomegaly with size ranging from 12 cm to 16 cm. Three of these patients had evidence of combined hepatosplenomegaly on imaging.
The upper gastrointestinal endoscopy (UGIE) was performed in seven patients. Three patients showed Grade I esophageal varices as evidence of portal hypertension. All of them showed extensive sinusoidal deposits on the biopsy. HVPG was done in one of case which was 7 mm of Hg.
In liver function tests most of patients had increased Serum Alkaline phosphate and Gamma-glutamyl transpeptidase levels. There was also reduction or reversal of A/G ratio. That might be due to either reduced albumin production from damaged hepatic parenchyma or due to primary globulin disorder. Serum Bilirubin was raised only in four patients. The serum creatinine was 1.1mg/dl (median). The hemoglobin, total leukocyte count and platelets were 11.4gm/dl, 11.4x10^9/l and 216x10^9/l (median) respectively. The International normalized ratio (INR) was 1.4 (median) (Table 2).
Other Organ Biopsies
The thirteen patients had undergone the other organ biopsies like Kidney, rectum, gastric antrum, duodenum, lung and heart. Kidney biopsy was done in three patients and two of them had amyloidosis. One of these patients was 54 years male who had M spike on serum electrophoresis. He died soon after starting the chemotherapy for Multiple Myeloma. His post-mortem kidney, liver & heart biopsy was done. All three biopsies showed extracellular homogenous eosinophilic material indicative of amyloidosis. Hence the diagnosis of primary amyloidosis with involvement of heart, kidney & liver was done.
Rectal biopsy was done in six patients and four biopsies were positive for amyloidosis. All the antral and duodenal biopsies (n=4) were negative for amyloidosis. One patient had undergone axillary lymph node biopsy which was positive for amyloidosis.
Bone Marrow Studies
Bone marrow studies composed of aspiration and biopsy were done in eleven patients. Eight patients showed marrow involvement by disease process, either due to plasma cell neoplasm or amyloidosis. Five biopsies showed amyloidosis with plasma cell neoplasm. Two biopsies had only amyloidosis. One of the biopsies showed evidence of plasma cell neoplasm without amyloidosis. The remaining three biopsies did not show either amyloidosis or plasma cell neoplasm. SAA immunostain on liver biopsy was positive in the two of these three cases. The liver biopsy in the third case was negative for all three immunostains.
Patterns of Amyloid deposition and immunohistochemistry (Table 3 and 4)
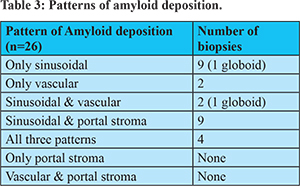
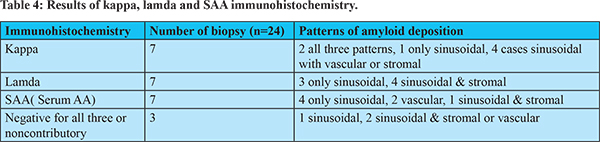
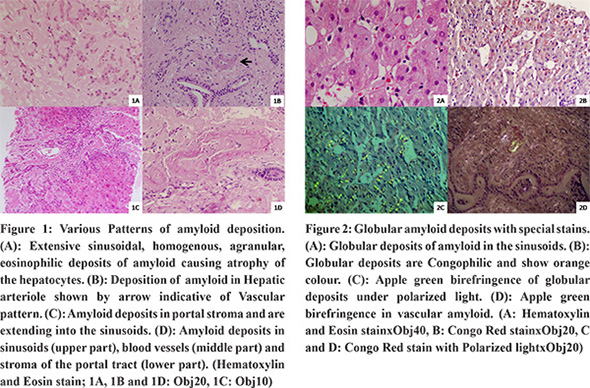
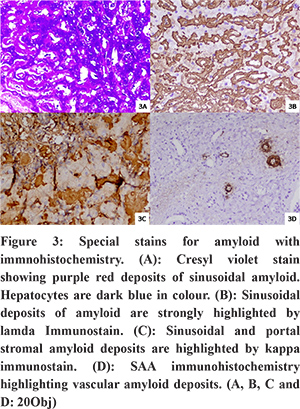
Amyloid material was deposited in sinusoids, portal stroma and blood vessels (Figure 1). In sinusoids amyloid deposits were linear or rarely globular. Congo Red staining was performed on all cases which showed congophilic material with Apple green birefringence on polarized light microscopy (Figure 2). Most common pattern of amyloid deposition was only sinusoidal and sinusoidal with portal stroma (n=9 in each group). All the thirteen patients with portal hypertension had sinusoidal deposits of amyloid. Amyloid deposits are purple red on Cresyl Violet staining. Kappa, lamda and SAA protein immunostains were performed. The two cases had only vascular amyloid deposition and both were positive for SAA immunohistochemistry (Figure 3). Three biopsies out of 24 of the patients were negative for all three immnostains. Other types of amyloid deposits like ATTR, A-beta etc can be suspected in these cases. One of three biopsies was female who had gastrointestinal and heart dysfunction due to amyloidosis as described previously.
Association with Hepatitis B
Three patients were positive for Hepatitis B surface antigen. IHC was available in two of them. Both were positive for Serum amyloid associated protein (SAA). One of them showed vascular and other showed globoid sinusoidal pattern. The third case showed sinusoidal deposits but immunohistochemistry cannot be performed due to technical problems.
Discussion
We had 26 cases of Hepatic amyloidosis diagnosed on biopsy. The clinical presentation, laboratory parameters and histological characters were studied. Most striking abnormality in the liver function tests was observed in levels of Serum alkaline phosphatase. Nineteen patients had elevated Serum alkaline phosphatase with median of 245 IU/L. Similar findings were seen in case series by Wang et al.1 Case reports have demonstrated elevated serum alkaline phosphatase levels11,12. The bone marrow examination was done in 10 out of these nineteen patients and nine of them showed marrow involvement by amyloid or plasma cell disorders. The cause of raised alkaline phosphatase cannot be ascertained. It can be due to bone involvement as seen in other hematological disorders or due to involvement of bile drainage system by amyloid.13
Bilirubin more than 2 mg/dl was seen in nine of 26 patients (34%). This is slightly higher than that found in the study done by the Park et al. They had 20 of 95 (21%) patients with bilirubin was greater than 34 micromol/L (2mg/dl).2 Simple explanation for increase in bilirubin could be mechanical damage to bile canaliculi and small sized bile ducts but this concept has been contradicted by ultrastuctural studies which do not show much change in these structures hence an alternative mechanism is suggested. Inhibition of Na-K ATPase pump or other functional damage to bile ductular epithelium is suggested.14
One of our patients with abdominal distention and cardiac arrest had hepatic amyloidosis. She had no ascites or portal hypertension. Autonomic nervous system dysfunction due to involvement by amyloidosis must have caused her to develop intestinal movement disorder leading to pseudoobstruction. Similarly cardiac dysfunction can also be explained. All the three immunohistochemistries were negative in her liver biopsy. The other types of material like Apo A1, transthyretin and Beta2 microglobulin may be have deposited in this case.15,16
The transabdominal liver biopsies are associated with increased risk of bleeding hence in high risk patients TJLBs were done.17 The TJLBs give privilege of measuring HVPG readings and doing biopsy in a single setting.
In our study the most common pattern of amyloid deposition was sinusoidal with or without portal stromal. The most common pattern in AA and non AA cases was sinusoidal pattern either as isolated or associated with some other form. This contrasted with the study published by Sarsik et al. They have vascular as most common pattern in approximately 91% patients of AA amyloidosis. In non AA amyloidosis mixed pattern was most common. In our study only 5 out of 24 patients had only sinusoidal pattern and rest all (84%) had sinusoidal with one or the other pattern. Sarsik et al also had mixed pattern as most common pattern in their study (72.7%).4
HVPG readings were available in twelve patients. Of these cases ten showed HVPG >6 mm of Hg indicating portal hypertension. All of them showed diffuse sinusoidal deposits of amyloid. The deposition of material in the space of Disse leads to reduction in the space of sinusoids and increases the resistance to blood flow leading to raised sinusoidal and in turn portal venous pressure. Thus sinusoidal deposits are main cause of portal hypertension in the hepatic amyloidosis.18 Similarly portal stromal deposits may lead to compression of the thin walled portal veins and further contribute to additional resistance to outflow.
Seven patients had undergone UGIE. Only three of them showed varices. Portosystemic shunts at lower end of esophagus lead to esophageal varices. Thus, they are secondary effect of the portal hypertension; hence they usually evolve over the certain time period. Similarly, if patient’s condition is rapidly deteriorating then these may get collapsed and difficult to visualize. This can explain the variable presence of varices in the cases of portal hypertension. Also the portal hypertension in the hepatic amyloidosis is associated with poor prognosis.18
All the five patients who had undergone transient elastography showed liver stiffness measurement of 75kPa. The fibroscan measures the stiffness that can be due to fibrosis, infiltration of the hepatic parenchyma by inflammation, amyloid material or due to neoplasm. Thus, these patients can be diagnosed as hepatic amyloidosis if there is some evidence of amyloidosis at other site of body. Loustaud et al showed liver stiffness more than 17.3 kPa indicates hepatic amyloidosis with non-fibrotic liver changes. Thus, transient elastography can be used as non invasive diagnostic tool in patients with known amyloidosis.19 However if fibroscan is not available then also the liver involvement can be diagnosed with updated non-invasive consensus diagnostic criteria for amyloid–related organ involvement. These guidelines provide noninvasive criteria for involvement of various organs like liver, heart, kidney etc in a known case of amyloid.20,21 However, amyloidosis is histological diagnosis. National Amyloidosis Center, London advocates the demonstration of amyloid in primary affected organ or in other biopsies like bone marrow or abdominal fat pad biopsy.17
To conclude, we are reporting the first large case series of Hepatic amyloidosis from a tertiary liver care center in India, to the best of our knowledge. The presenting complaints, laboratory parameters, HVPG, histopathological and immunohistochemical properties were studied. Further larger studies with long term follow up will help in better understanding of the disease pathology and its progression which may help in future in treating the underlying cause with special care to avoid further liver damage and help in prolonging survival of patients.
References
- Wang YD, Zhao CY, Yin HZ. Primary hepatic amyloidosis: a mini literature review and five cases report. Annals of hepatology. 2012;11(5):721-7.
- Park MA, Mueller PS, Kyle RA, Larson DR, Plevak MF, Gertz MA. Primary (AL) hepatic amyloidosis: clinical features and natural history in 98 patients. Medicine. 2003;82(5):291-8.
- Naito KS, Ichiyama T, Kawakami S, Kadoya M, Tabata T, Matsuda M, et al. AL amyloidosis with spontaneous hepatic rupture: successful treatment by transcatheter hepatic artery embolization. Amyloid : the international journal of experimental and clinical investigation : the official journal of the International Society of Amyloidosis. 2008;15(2):137-9.
- Sarsik B, Sen S, Kirdok FS, Akarca US, Toz H, Yilmaz F. Hepatic amyloidosis: morphologic spectrum of histopathological changes in AA and nonAA amyloidosis. Pathology, research and practice. 2012;208(12):713-8.
- Gertz MA, Kyle RA. Hepatic amyloidosis: clinical appraisal in 77 patients. Hepatology. 1997;25(1):118-21.
- Kennedy PA, Madding GF. Surgical anatomy of the liver. The Surgical clinics of North America. 1977;57(2):233-44.
- Benter T, Kluhs L, Teichgraber U. Sonography of the spleen. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2011;30(9):1281-93.
- Frank K, Linhart P, Kortsik C, Wohlenberg H. [Sonographic determination of spleen size: normal dimensions in adults with a healthy spleen]. Ultraschall in der Medizin. 1986;7(3):134-7.
- Gadano A, Hadengue A, Widmann JJ, Vachiery F, Moreau R, Yang S, et al. Hemodynamics after orthotopic liver transplantation: study of associated factors and long-term effects. Hepatology. 1995;22(2):458-65.
- Navasa M, Feu F, Garcia-Pagan JC, Jimenez W, Llach J, Rimola A, et al. Hemodynamic and humoral changes after liver transplantation in patients with cirrhosis. Hepatology. 1993;17(3):355-60.
- Shin YM. Hepatic amyloidosis. The Korean journal of hepatology. 2011;17(1):80-3.
- Sonthalia N, Jain S, Pawar S, Zanwar V, Surude R, Rathi PM. Primary hepatic amyloidosis: A case report and review of literature. World journal of hepatology. 2016;8(6):340-4.
- Murakami J, Shimizu Y. Hepatic manifestations in hematological disorders. International journal of hepatology. 2013;2013:484903.
- Peters RA, Koukoulis G, Gimson A, Portmann B, Westaby D, Williams R. Primary amyloidosis and severe intrahepatic cholestatic jaundice. Gut. 1994;35(9):1322-5.
- Shin SC, Robinson-Papp J. Amyloid neuropathies. The Mount Sinai journal of medicine, New York. 2012;79(6):733-48.
- Wang AK, Fealey RD, Gehrking TL, Low PA. Patterns of neuropathy and autonomic failure in patients with amyloidosis. Mayo Clinic proceedings. 2008;83(11):1226-30.
- Gillmore JD, Wechalekar A, Bird J, Cavenagh J, Hawkins S, Kazmi M, et al. Guidelines on the diagnosis and investigation of AL amyloidosis. British journal of haematology. 2015;168(2):207-18.
- Bion E, Brenard R, Pariente EA, Lebrec D, Degott C, Maitre F, et al. Sinusoidal portal hypertension in hepatic amyloidosis. Gut. 1991;32(2):227-30.
- Loustaud-Ratti VR, Cypierre A, Rousseau A, Yagoubi F, Abraham J, Fauchais AL, et al. Non-invasive detection of hepatic amyloidosis: FibroScan, a new tool. Amyloid : the international journal of experimental and clinical investigation : the official journal of the International Society of Amyloidosis. 2011;18(1):19-24.
- Gertz MA, Comenzo R, Falk RH, Fermand JP, Hazenberg BP, Hawkins PN, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18-22 April 2004. American journal of hematology. 2005;79(4):319-28.
- Gertz MA MG. Definition of organ involvement and response to treatment in AL amyloidosis: an updated consensus opinion. Amyloid : the international journal of experimental and clinical investigation : the official journal of the International Society of Amyloidosis. 2010(17(Suppl 1)):48–9.