48uep6bbphidcol2|ID
48uep6bbphidvals|2987
48uep6bbph|2000F98CTab_Articles|Fulltext
Extra-pulmonary tuberculosis (EPTB) is often misdiagnosed, mistreated or underestimated because of the nonspecific clinical manifestations as well as the lack of familiarity with protean presentations.1 We have recently had the opportunity of observing a teachable case of EPTB.
A 46-year-old gentleman presented with epigastric mass and abdominal distension of three months duration along with intermittent fever, anorexia, and weight loss. Physical examination revealed left supraclavicular lymphadenopathy, a slightly tender epigastric mass, moderate hepato-splenomegaly, and a tense ascites. The clinical possibility of malignant etiologies such as metastatic gastrointestinal cancer and high-grade lymphoma were kept by the MD resident during the bedside case presentation in the ward rounds.
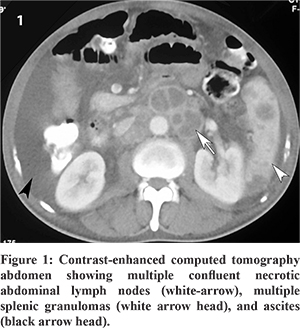
Basic laboratory investigations showed bicytopenia (hemoglobin 98 g/L, thrombocytopenia 63×109/L), high blood sugars and cholestatic liver injury pattern (total and conjugated bilirubin, 44.46 and 22.57 µmol/L respectively; aspartate aminotransferase, alanine aminotransferase and alkaline phosphatase of 1.54 µkat/L, 0.85 µkat/L, and 8.28 µkat/L respectively). Fine needle aspiration cytology (FNAC) from the left supraclavicular node showed acid-fast bacilli and extensive necrosis. Subsequently, a computed tomography of chest and abdomen showed enlarged necrotic lymph nodes in neck, mediastinum, retroperitoneum, and periportal location; hypodense lesions in spleen and left adrenal; mild ileocaecal thickening; gross ascites; and few nodules in the left upper lobe of the lung (Figure 1). The ascitic fluid examination did not reveal malignant cells. With a diagnosis of disseminated tuberculosis and diabetes mellitus, the patient was started on anti-tubercular treatment and metformin. Four weeks into the treatment, the patient improved significantly.
All Virchow’s node, abdominal mass, and ascites are not always malignancy; tuberculosis may be a mimic. Lymphadenitis is the most common form of the EPTB. Cervical lymph nodes (particularly posterior chain) are the most commonly affected. Supraclavicular lymphadenopathy is uncommon. FNAC is a minimally invasive procedure and gives an excellent bacteriological yield.2
References
- Raut AA, Naphade PS, Ramakantan R. Imaging Spectrum of Extrathoracic Tuberculosis. Radiol Clin N Am 2016;54(3):475–501.
- Schaaf HS, Zumla A, ed. Tuberculosis. A comprehensive clinical reference. 1st ed. Saunders: Elsevier, 2009, pp.391-95.