48uep6bbphidcol2|ID
48uep6bbphidvals|2984
48uep6bbph|2000F98CTab_Articles|Fulltext
Basidiobolomycosis is a rare fungal infection caused by Basidiobolus ranarum.1 The most frequent site of infection is the subcutaneous areas, of young males, with transmission due to trauma or insect bites.2 The tropics have the highest number of reported cases. Clinically it is difficult to diagnose gastrointestinal (GI) basidiobolomycosis, as there are no specific signs and symptoms described.3 We report a young Kurdish gentleman with a lesion in the transverse colon, which was found to be basidiobolomycosis on histopathologic examination.
Case Report
A 26-year Kurdish gentleman presented with dull aching abdominal pain, nausea, vomiting, weight loss, and loss of appetite. Clinically he was stable with no palpable abdominal lump.
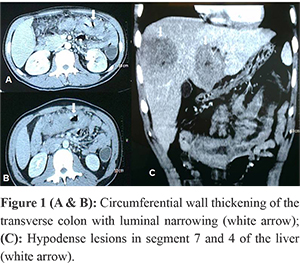
His laboratory profile was normal except for leucocytosis and peripheral eosinophilia. He was detected to be hepatitis B antigen positive, with normal liver function tests and albumin. Abdominal ultrasonography (USG) showed thickening of the transverse colon. Computed Tomography (CT) scan of the abdomen showed circumferential thickening of the mid-distal transverse colon with luminal narrowing and few pericolic nodes (Figure 1A & 1B). In the portal venous phase, two hypodense lesions with irregular walls in segments 7 and 4 of the liver were seen (Figure 1C). There was no ascites or peritoneal lesions. The possibilities of colonic malignancy versus lymphoma were raised. The pathologist in Kurdistan had raised a possibility of fungal infiltrates in the colonoscopic biopsy. A repeat colonoscopy with us revealed an incomplete stricture of the middle and distal transverse colon with mucosal ulceration, a biopsy of which showed inflammatory cells.
The patient was subjected to laparotomy. On exploration, the distal transverse colon was thickened with luminal narrowing (Figure 2A & 2C) and a few nodes in the mesocolon. There were these dusky lesions in segment 4 (Figure 2B) and 7 of the liver. He underwent transverse colectomy with stapled side to side colocolic anastomosis. He required secondary suturing for burst abdomen on the 6th post day.
On histological examination, the sections from the stricture area showed transmural infiltrates of eosinophils, neutrophils, and lymphocytes with eosinophilic abscesses (Figure 3A & 3B). Multiple granulomas composed of eosinophils, lymphocytes, epithelioid cells & multinucleate giant cells were present (Figure 3C). These filaments were broad, thin-walled & septate (Figure 3D). Many places showed Splendore-Hoeppli phenomenon, i.e., fungal filaments surrounded by dense infiltrates of eosinophils (Figure 3C & 3D). These features were suggestive of basidiobolomycosis.
He was prescribed daily oral itraconazole (200 mg) for two years.On e-mail follow-ups, he remains asymptomatic and is in good health for the last four years. His follow up ultrasound showed regression of liver lesions.
Discussion
Basidiobolomycosis is a rare fungal infection caused by the fungus Basidiobolus ranarum.1 This infection is seen predominantly in the tropics, producing chronic subcutaneous infection in the extremities.2 There is a paucity of literature regarding GI tract involvement, with a few cases reported of colonic basidiobolomycosis. Fatal infections causing systemic sepsis have been reported.4 The mode of transmission is unclear, but the faeco-oral route is believed to be the reason for gastrointestinal infections.3
Clinically and radiologically, it is difficult to differentiate GI basidiobolomycosis from inflammatory bowel disease or malignancy. GI basidiobolomycosis is often associated with leucocytosis and eosinophilia. These lab parameters respond after surgical resection of the lesion, as was noticed in our patient.
Preoperatively, we made a differential diagnosis of malignancy or lymphoma of the colon. Inflammatory bowel disease is a common pitfall while diagnosing. The difficulty in diagnosing this condition is due to several reasons. Firstly, the non-specific clinical presentation with no known risk factors described.3 Secondly, colonoscopic biopsies may not help as often they are superficial, and the causative organism lies deep beneath the mucosa. A biopsy on biopsy or well biopsy may help to clinch the diagnosis. More often, the biopsy reveals non-specific inflammation or inflammatory cells, as was seen in our case. In our case, the pathologist from Kurdistan had raised suspicion of fungal infiltrates. We were unaware of this entity and always thought of either carcinoma or lymphoma of the colon due to its colonoscopic picture and CT scan image. If there is a high index of suspicion, the tissue can be sent for fungal culture.5 The third reason is that these patients are healthier compared to patients with opportunistic fungal infections who are sick and immunocompromised. The fourth reason being, isolated lesions without any systemic involvement, makes serological tests useless for diagnosis.
These patients are subjected to surgical resection of the involved colonic segment due to difficulty in pre-operative diagnosis. Once diagnosed, these patients are placed on prolonged oral antifungal therapy. The correct diagnosis is made by the histopathological examination of the resected specimen or by isolating the particular organism from the cultured tissues.3 Histologically, there are fungal hyphae, necrotic areas, eosinophilic and lymphocytic infiltrates. Splendore-Hoeppli phenomenon is seen, which consists of broad, thin-walled fungal hyphae & surrounding eosinophils forming eosinophilic abscess.5 The involved bowel segment shows marked mural thickening, fibrosis, prominent eosinophilic infiltration, and granulomatous reaction. All these features were present in our case and helped us to discover the true nature of the pathology. Due to a lack of suspicion, we failed to carry out tissue culture in our case. Serological tests by detecting specific antibodies also can be used to confirm the diagnosis and monitor the response to treatment.3
All the azoles (fluconazole, itraconazole, ketoconazole, miconazole) have been found to be equally effective against the Basidiobolus species.6 The duration of antifungal therapy is not clearly described, but often a prolonged treatment for up to 6 months to 2 years is given.7 There is conflicting data about the effectiveness of potassium iodide. Response to therapy is judged by documenting the regression of the lesions on CT scan or by noticing the disappearance of specific antibodies on serological tests.3 In our patient, USG revealed a regression of the liver lesions.
Conclusion
In the case reported here, there was no pre-operative suspicion, and the histological report surprisingly showed features of basidiobolomycosis. GI basidiobolomycosis is now a recognized disease. The clinical features mimic inflammatory or malignant bowel disease. Basidiobolomycosis should be considered in the list of differential diagnosis in young patients with atypical colonic lesions from the middle-east. An experienced pathologist and a high index of suspicion are required to make the correct diagnosis.
References
- Dixon DM, Fromtling R A. Manual of Clinical Microbiology. 6th ed, Washington DC USA, ASM press; 1995, 699–708.
- Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatment. ClinMicrobiol Infect. 2004; 10 (suppl. 1): 31–47.
- Lyon GM, Smilack JD, Komatsu KK, PashaTM, LeightonJA, GuarnerJetal. Gastrointestinal basidiobolomycosis in Arizona: clinical and epidemiological characteristics and review of the literature. Clin Infect Dis. 2001 May 15;32(10):1448-55
- vandenBerk GE, Noorduyn LA, vanKetel RJ, van Leeuwen J, Bemelman WA, Prins JM. A fatal pseudotumour: disseminated basidiobolomycosis. BMC Infect Dis. 2006 Sep 15; 6:140.
- Nemenqani D, Yaqoob N, Khoja H, AlSaif O, Amra NK, AmrSS..Gastrointestinal Basidiobolomycosis: an unusual fungal infection mimicking colon cancer. Arch Pathol Lab Med. 2009 Dec;133(12):1938-42
- Guarro J, Aguilar C, Pujol I. In-vitro antifungal susceptibilities of Basidiobolus and Conidiobolus spp. Strains. J Antimicrob Chemother. 1999 Oct;44(4):557-60
- Saka B, Kombaté K, Mouhari-Toure A, Akakpo S, Tchangaï B, Amégbor K etal. Probable basidiobolomycosis in a Togolese rural young successfully treated with ketoconazole. Bull SocPatholExot. 2010 Dec;103(5):293-5.