48uep6bbphidcol2|ID
48uep6bbphidvals|2972
48uep6bbph|2000F98CTab_Articles|Fulltext
It is well known that acute pancreatitis can be complicated by renal failure due to various mechanisms. In most cases, acute renal failure is due to acute tubular necrosis, and kidneys recover entirely with supportive care1. However, acute renal cortical necrosis complicating acute pancreatitis is a rare event, and recovery is unlikely. Only a few cases are reported in the literature. We present a case of acute necrotizing pancreatitis complicated by the rare complication of acute renal cortical necrosis, showing characteristic imaging features.
Case Report
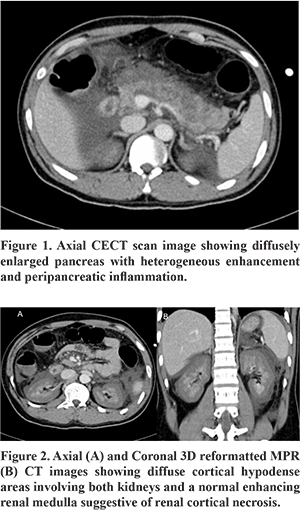
A 30-year-old male with no previous illness presented to trauma center with a history of road traffic injury. The airway was patent, breathing and circulation were normal. Glasgow Coma Score (GCS) was 15. On physical examination, there was tenderness in the epigastrium. Focused assessment with sonography in trauma (FAST) was positive for free fluid in Morrison’s pouch and pelvis. CECT torso was performed, which showed diffuse enlargement of the pancreas with heterogeneous enhancement and peripancreatic inflammation (Figure 1). Also, Bilateral kidneys showed diffuse cortical hypodense areas and a normal enhancing renal medulla suggestive of renal cortical necrosis (Figure 2). Subsequently, laboratory investigations revealed raised serum creatinine (5mg/dl) and amylase (700 U/L) levels. Over the next three days, the patient developed anuria. He received supportive management, antibiotics, and dialysis support. He is being evaluated for renal transplantation since there was no improvement in renal function during the hospital course.
Discussion
A serious complication of severe acute pancreatitis is acute renal failure, an important indicator of morbidity and mortality in critically ill patients.
Acute renal failure may result from various mechanisms such as hypoxemia, impaired renal perfusion, the release of pancreatic enzymes from the inflamed pancreas causing damage to renal microcirculation, or abdominal compartment syndrome. Other possible theories, such as the release of endotoxins and reactive oxygen species, have been implicated in the pathophysiology of renal injury2.
Bilateral cortical necrosis is a rare complication of severe acute pancreatitis; only a few cases of bilateral cortical necrosis following acute pancreatitis were reported in the literature. Cortical necrosis commonly results from reduced perfusion within microcirculation of the renal cortex following septic shock or hypovolemia. However, the cause remains mysterious in normotensive patients, is ascribed due to the release of vasoactive or cytotoxic substances during pancreatitis3.
Imaging features are characteristic; contrast-enhanced CT shows a non-enhancing renal cortex and a normal enhancing renal medulla described as reverse rim sign4. Sometime, a very thin rim of contrast enhancement i.e., cortical rim sign, may be seen and should not be mistaken for adequate perfusion5. These imaging features correlate with the death of all cells in the cortex and congestion of the medulla on histology1,6. The capsule and a thin rim of the peripheral cortex (1-2 mm) are spared because of its separate capsular blood supply7.
In the majority of the cases, acute renal failure is due to acute tubular necrosis, and kidneys recover completely with supportive care. However, acute renal cortical necrosis complicating acute pancreatitis is a rare event, and recovery is unlikely.
The prognosis is very poor, nearly most end up in renal replacement therapy after a variable period. The majority of patients with the diffuse type of cortical necrosis will not recover renal function, while patients with patchy cortical necrosis may show some improvement in renal function but gradually develop the end-stage renal disease and only curative treatment is renal transplantation8.
References
- Anandan AK, Balachandran P, Chowksey A, Sankaranarayanan G, Samuel U. Bilateral renal cortical necrosis following acute pancreatitis - A rare complication of a common disease. Saudi J Kidney Dis Transpl 2018; 29:1211-5.
- Petejova N, Martinek A. Acute kidney injury following acute pancreatitis: A review. Biomed Pap Med FacUnivPalacky Olomouc Czech Repub. 2013 Jun;157(2):105-13.
- Krishna GS, Kishore KC, Sriram NP, Sainaresh VV, Lakshmi AY, Siva Kumar V. Bilateral renal cortical necrosis in acute pancreatitis. Indian J Nephrol. 2009 Jul;19(3):125.
- Thuysbaert T, Standaert C, De Visschere P. Reverse Rim Sign. J Belg Soc Radiol. 2018 Feb 14;102(1):27.
- Dyer RB, Chen MY, Zagoria RJ. Classic signs in uroradiology. Radiographics. 2004 Oct;24 Suppl 1:S247-80. Review.
- Badiola-Varela CM. Acute renal cortical necrosis: contrast-enhanced CT and pathologic correlation. UrolRadiol. 1992;14(3):159-60
- Goergen TG, Lindstrom RR, Tan H, Lilley JJ. CT appearance of acute renal cortical necrosis. AJR Am J Roentgenol. 1981 Jul;137(1):176-7.
- Chugh KS, Jha V, Sakhuja V, Joshi K. Acute renal cortical necrosis – A study of 113 patients. Ren Fail 1994;16:37-47.