48uep6bbphidcol2|ID
48uep6bbphidvals|2947
48uep6bbph|2000F98CTab_Articles|Fulltext
Marathon runners are prone to dehydration, muscle cramps, rhabdomyolysis, and heatstroke. Rarely, long running has been mentioned in literature as a cause for acute pancreatitis, but to the best of our knowledge, no case has been reported from India to date. Here we report a case of acute pancreatitis following a marathon run after ruling out all possible aetiologies.
Case Report
Our patient was a 20-year-old male who presented in the emergency department in evening hours with complaints of severe epigastric pain radiating to back, three to four episodes of vomiting, and an inability to pass motion and flatus since the same day morning. The pain started when he was running a marathon and had already completed 12 kilometres (km) within four hours. His pace was nearly three km/hr. After running for the next half kilometre, he had to quit the marathon because of increased severity of pain and had to take a cab for his home. According to him, his fluid intake was less that day. There was no history of alcohol abuse or drug ingestion, abdominal trauma, endoscopic intervention, jaundice, or any comorbidities. There was no history of a similar type of pain in the past. There was no history suggestive of peptic ulcer disease. There was no family history of pancreatitis or hyperlipidaemia. On examination, he had tachycardia, normal blood pressure, and his spO2 was normal. He was dehydrated and had tenderness all over the abdomen with decreased bowel sounds. There was no guarding, no rigidity, no organomegaly, no flank dullness. He was admitted and investigated.
His serum amylase and lipase levels were elevated more than eight and ten times, respectively (924 U/L/ 4268 U/L, respectively) (reference range for Amylase 25-115 U/L, Lipase 73-393 U/L). CRP was also raised (78.8 mg/L) (reference range 0.0-5.0 mg/L). LFT, RFT, and Thyroid profile were within the normal range. CBC was showing increased WBC count (19770/mm3). USG abdomen was showing hypoechoic and bulky pancreas with evidence of fluid collection in the peri-pancreatic region of size 90 cc approximately, mild hepatomegaly, and minimal left-sided pleural effusion, with no gall stones or gall bladder (GB) sludge, findings suggestive of acute pancreatitis. He was started on standard protocol for the treatment of acute pancreatitis. He underwent extensive workup to rule out the common and uncommon causes of AP, but no aetiology could be confirmed. His serum calcium and lipid profile were within the normal range.
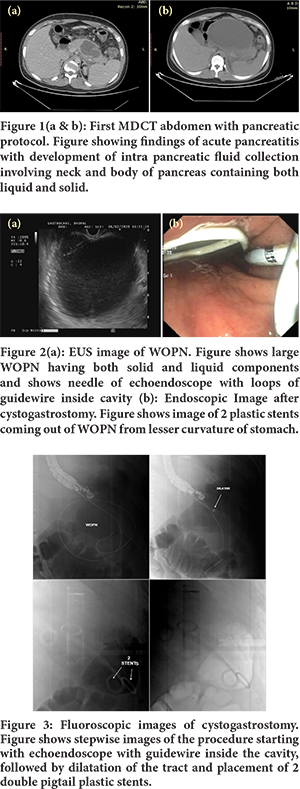
His MDCT abdomen with the pancreatic protocol was showing bulky heterogeneously enhancing pancreas with intra-pancreatic fluid collection involving the neck and proximal body regions with multiple extra pancreatic fluid collections involving both pleural spaces, peri-gastric, peri-splenic, infra-pancreatic, para-colic and pelvic regions suggestive of acute necrotizing pancreatitis with CT severity index of 8. (Figure 1a) He was managed initially conservatively. His initial haematocrit was 42.6%, which improved to 35.1%. Repeat MDCT abdomen with the pancreatic protocol was suggestive of acute necrotizing pancreatitis with an increased size of collections compared to the previous one. (Figure 1b) During his second hospitalization, he was found to have large WOPN, which became symptomatic in the form of increased abdominal pain and unable to tolerate food and fluids, which required drainage in the form of endoscopic cystogastrostomy. (Figure 2,3) Later he did well, and now he is asymptomatic and in regular follow up.
Discussion
Abdominal pain frequently occurs after long-distance running. Proposed mechanisms are diaphragmatic ischemia, dehydration, muscular spasm, or myonecrosis.1 Acute pancreatitis had also been described in the literature to occur after prolonged strenuous exercise in the form of a marathon, but there is no consensus upon its exact pathophysiology. Many mechanisms had been proposed for its occurrence. Ischemia due to low blood flow secondary to the diversion of the majority of blood flow to muscles, ischemia due to dehydration leading to hypovolemia and repetitive mechanical trauma to the pancreas against posterior abdominal wall and spine after prolonged running had been few of them.1-3 It is more common in more dehydrated patients and those who had travelled more distance. Systemic stress leading to direct damage to the pancreas had also been proposed as one of the mechanisms based upon animal studies.4 No mention had been found about the role of speed of traveling, posture while running, and weather conditions in its development. Our patient probably had a variable combination of above all mechanisms suggesting marathon running as the cause for his acute pancreatitis as he was an untrained marathon runner, had a long run for the first time, was fasting, not properly hydrated during the run and had elevated haematocrit suggestive of dehydration in the absence of other risk factors.
The pancreas is known to be susceptible to ischemia, and there is a consensus that it plays a primary role in acute pancreatitis development.5 Hypoperfusion of the pancreatic tissue results in cell necrosis and leukocyte infiltration due to hypo-oxygenation and endothelial dysfunction, respectively. The endothelial wall becomes more permeable, and O2 radicals formed by leukocyte activation exacerbate the process of acute pancreatitis. In many situations, reperfusion alone may not reverse the necrotic process and may even worsen pancreatitis by inducing the formation of O2 radicals.6
Thus, it can be said that acute pancreatitis can be prevented in marathon runners by maintaining proper hydration by taking fluids before, during, and after the run and by educating them to stop after the development of even slightest abdominal pain. They should also load themselves with carbohydrates day before the event and continue to take carbohydrates before, during, and after run in the form of liquid drinks enriched with carbohydrates at least for races lasting more than 60 minutes and should follow standard nutritional advice. Thus it becomes imperative that they should go through proper training before attempting a long run.7
Conclusion
Acute pancreatitis can develop in marathon runners, with ischemia being the most likely explanation. This case highlights that acute necrotizing pancreatitis should be considered as a differential diagnosis in a particular clinical context.
Financial Support and sponsorship: Nil.
Conflicts of Interest: There are no conflicts of interest.
References
- Stewart D, Waxman K. Marathon pancreatitis: is the aetiology repetitive trauma? Am Surg 2004; 70:561-3.
- Raper SE. Acute pancreatitis secondary to dehydration: case report and review of the literature. Am Surg 1999; 65:1084-7
- Mast JJ, Morak MJ, Brett BT, et al. Ischemic acute necrotizing pancreatitisin a marathon runner. J Pancreas. 2009; 10(1):53–54.
- Takano S, Kimura T, Kawabuchi M, et al. Ultrastructural study of the effects of stress on the pancreas in rats. Pancreas 1994; 9:249-57.
- Sakorafas GH, Tsiotos GG, Sarr MG. Ischemia/Reperfusion- Induced pancreatitis. Dig Surg 2000; 17:3-14.
- Cuthbertson CM, Christophi C. Disturbances of the microcirculation in acute pancreatitis. Br J Surg 2006; 93:518-30.
- Burke LM. Nutrition Strategies for the Marathon. Sports Medicine 2007; 37: 344-344.