|
Pravir Gambhire1, Ravi Thanage1, Ashok Mohite1, Vinay Zanwar1, Sreelakshmi Vaidyanathan2, Samit Jain1, Alka Subramanyam2, Pravin Rathi1 1Department of Gastroenterology, 2Department of Psychiatry, TNMC and B.Y.L Nair Hospital, Mumbai, India.
Corresponding Author:
Dr Pravir Gambhire Email: svpnavodaya@gmail.com
Abstract
Background: Irritable bowel syndrome (IBS) is a chronic condition. Some patients may benefit from probiotics and rifaximin in diarrhea-predominant IBS (IBS-D). Relaxation therapy has also been tried. Aims and Objectives: To assess the efficacy of rifaximin, VSL#3, and relaxation therapy in IBS-D patients. Methods: 196 patients with IBS-D were randomly assigned to three groups. Group A, B, and C received rifaximin, VSL#3, and relaxation therapy, respectively. Patients were followed up for six months. Results: Relaxation therapy (2.69 ± 0.67) group had significantly improved generalized ill-feeling over VSL# (3.87 ± 0.34) at the end of 6 months. IBS severity score improved in all the groups till the end of the study but relaxation therapy (199.19 ± 30.02) was significantly better than rifaximin (217.21 ± 39.9) and VSL# (250.41 ± 14.78). The subjective global assessment was improved significantly in the relaxation therapy group (2.05 ± 0.9) as compared to rifaximin (3.02 ± 0.85) and VSL#3 (3.84 ± 0.37). Conclusion: Patients with IBS-D do better with rifaximin and VSL#3 in the short term. Patients respond better to relaxation therapy at the end of 6 months. Relaxation therapy is being a non-pharmacological and cost-effective therapy, could be implemented on a long-term basis.
|
48uep6bbphidcol2|ID 48uep6bbphidvals|1940 48uep6bbph|2000F98CTab_Articles|Fulltext Introduction
The Rome III criteria define irritable bowel syndrome (IBS) as a chronic disorder characterized by abdominal pain or discomfort associated with disordered defecation either constipation (IBS-C), diarrhea (IBS-D) or mixed/alternating symptoms of constipation and diarrhea (IBS-M).1 Rome IV omitted abdominal discomfort from the definition. In a study from India, the prevalence of IBS was reported to be 4%.2 IBS reduces patients’ quality of life. Bloating and abdominal distension are frequently reported by patients reflecting increased sensitivity to normal amounts of intestinal gas.3 The overgrowth of microbiota in the small intestine can cause excessive gas production and malabsorption with a variety of nonspecific symptoms, such as diarrhea, gas bloating, abdominal pain, and constipation.4 There may be benefits of the antibiotic rifaximin demonstrated by efficacy and durable improvement in symptoms.5 Rifaximin demonstrates no clinically relevant bacterial resistance because less than 0.5% of the oral dose is absorbed. These features make rifaximin acceptable for repeated courses of treatment.6,7 Probiotics reinforce the intestinal mucosal barrier and normalize the digestive tract’s motility and visceral sensitivity. Some lactobacilli strains may modulate intestinal pain attacks by inducing the expression of µ-opioid and cannabinoid receptors in the intestinal epithelial cells.8 The most widely prescribed probiotic, that is used in most of the trials is a molecule of VSL#3, which contains eight strains of lactic acid bacteria (Streptococcus thermophilus, Bifidobacteriumbreve, Bifidobacteriumlongum, Bifidobacteriuminfantis, Lactobacillus acidophilus, Lactobacillus plantarum, Lactobacillus paracasei and Lactobacillus delbrueckii (subspecies bulgaricus). The relationship between the neural and immunological networks within the gut and the bi-directional communication between the gut and the central nervous system (CNS) is referred to as the brain-gut axis (BGA).9 Structural and functional disruptions in the BGA cause changes in perceptual and re?exive responses of the nervous system that may lead to gastrointestinal disorders, like IBS.10 Psychotherapy primarily relieves symptoms by helping the patient face underlying psychological conflicts and emotional disturbances. In a landmark study, Svedlund J et al. reported that the psychotherapy group showed significantly more significant improvement than the controls on measures of abdominal pain, bowel dysfunction, and mental symptoms.11 In this study, we assess the efficacy of rifaximin, VSL#3, and relaxation therapy in patients of IBS-D. Its effect on generalized ill-feeling, IBS Severity Score (IBS SS), and Subjective Global Assessment (SGA) was studied over six months. The effect of these therapies on the quality of life was also compared.
Method
Study Design: It was a comparative parallel prospective open-labelled randomized study. The Institutional Ethics Committee approved the protocol before implementation at the site.
Inclusion Criteria: Patients aged 18 to 65 years with a diagnosis of IBS (D) as per Rome III criteria and moderate severity according to IBS Severity Score (IBSSS) were included in the study.
Exclusion Criteria: Patient having occult or overt blood in stools; a history of colon cancer, inflammatory bowel disease, or celiac disease; night-time symptoms (awakening the patient from sleep); patients who are immunocompromised; patients with significant weight loss (>10% of body weight), anemia (<13 g/dl in males and <11 g/dl in females); ingesting probiotics or prebiotics in the two weeks preceding the study; antibiotic intake in last three months; pregnant and lactating females; using hormonal contraception; psychiatric disease on baseline evaluation; who have recently ( within 3 months) initiated the dietary measures (FODMAP diet)12 to control IBS symptoms.
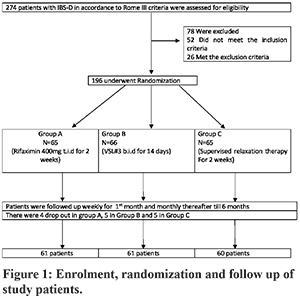
Methodology: Patients were recruited from the gastroenterology outpatient clinic after baseline evaluation and psychiatric examination as per the inclusion and exclusion criteria (Figure 1). The severity of IBS symptoms was rated using IBSSS.13 One hundred and ninety-six patients were randomly assigned to 3 treatment groups (Figure 1). The baseline characteristics of the treatment groups were similar. The quality of life (QOL) was assessed using a seven-point Likert scale.14 All patients received therapy for two weeks. Group A received rifaximin 400 mg thrice daily, Group B received VSL#3 twice daily, and Group C received relaxation therapy by the psychiatrist. Thereafter, patients were interviewed at weekly intervals for one month, followed by monthly for six months. Patients on medications were told to bring the empty packets while on weekly follow up to ensure compliance. In the relaxation therapy group, compliance was ensured by a counsellor by telephonic reminders weekly, and during the monthly follow up until the end of the study. Relaxation therapy consisted of 20-minute sessions, supervised four times during the two week study period. Patients were taught Jacobson’s classical progressive muscle relaxation techniques and were told to do it regularly for 20 minutes a day on awakening or before retiring. Progressive relaxation involved tensing and relaxing, in succession, sixteen different muscle groups of the body, including jaw, neck, shoulder, upper and lower back, chest, abdomen, hip, thighs, knees, calf, and ankle. Each muscle group had to be tensed for about 10 seconds and then suddenly let go. The patient then gives himself 15-20 seconds to relax. The data was organized and analysed by ratification on scales to gauge whether and how it was in accordance with the aims and objectives of the study.
Tools Used:
1. Seven-point Likert Scale: 0 = never, 1 = almost never, 2 = seldom, 3 = sometimes, 4 = often, 5 = almost always, 6 = always 2. Subjective global assessment (SGA) score: 1 = completely relieved, 2 = considerably relieved, 3 = somewhat relieved, 4 = unchanged and 5 = worse. 3. IBS Severity Score (IBSSS) (Table 1) We calculated that we would need to enrol 163 patients in order to detect a reduction in the rate of the composite primary endpoint with a power of 80% and a two-sided alpha level of 0.05.
Data Analysis and Statistical Methods Used:
The randomization of study participants was done by the research randomizer software. Qualitative data was represented in the form of frequency and percentage. Association between qualitative variables was assessed by Chi-Square test with ContinuityCorrection for all 2 X 2 tables and with or without Continuity Correction in the rest and Fisher’s exact test for all 2 X 2 tables where p-value of the Chi-Square test was not valid due to small counts. Before and after comparison of Qualitative data within each group was done using the McNemar Test. Quantitative data was represented using Mean±SD and Median and Interquartile range (IQR). Analysis of Quantitative data between a qualitative variable between 3 groups was done using One-way ANOVA if data passed ‘Normality test’ and by Kruskal-Wallis test if data failed ‘Normality test’, with the application of appropriate Post Hoc test if the p-value of ANOVA came statistically significant. Relationship between Quantitative data was assessed usingPearson’s Correlation if data passed ‘Normality test’ and by Spearman’scorrelation if data failed ‘Normality test’. SPSS Version 17 was used for mostanalysis.
Results
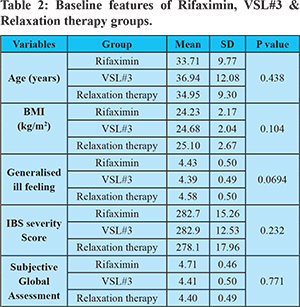
Enrolment, randomization, and follow-up are shown in Figure 1. Of the 196 patients enrolled, 182 completed the study; four patients in the rifaximin group, five patients in the VSL#3, and five patients in the Relaxation therapy group were lost to follow up. Three patients in each of the rifaximin and VSL#3 groups and two in the Relaxation therapy group felt improved with the therapy and quit in the first and third months, respectively; the rest of the patients were lost to follow up. The maximum percentage drop out was 7.69 %, and differential percentage drop out rate was1.54%. Baseline characteristics of the study population are shown in (Table 2). Male represented 55% of study participants, the mean age of the study population was 35.2 years (±10.4years).
Comparison of generalized ill-feeling between rifaximin, VSL#3 and relaxation therapy groups: From the first month of follow-up; the difference was significant among the three groups. At the end of the first and third month, rifaximin was better than VSL#3 and relaxation therapy; VSL#3 was better than relaxation therapy. At the end of sixth month rifaximin (3.07 ± 0.54) and relaxation therapy (2.69 ± 0.67) showed significant improvement than VSL#3 (3.87 ± 0.34), but the difference between rifaximin and relaxation therapy was not significant. [Table 3(A, B)]
Comparison of IBS Severity Score between rifaximin, VSL#3 and relaxation therapy: From the first month of followup, the difference was significant among three groups. By pairwise comparisons, rifaximin was better than VSL#3 and relaxation therapy until six months.[Table 4(A,B)] At 6 months, relaxation therapy (199.19 ± 30.02) was significantly better than rifaximin (217.21 ±39.93) and VSL#3 (250.41 ± 14.78).
Comparison of SGA for relief between rifaximin, VSL#3 and relaxation therapy: SGA score took time to improve. The difference was significant among the three groups at the end of the sixth month. Bypairwise comparisons, relaxation therapy (2.05 ± 0.9) was significantly better than rifaximin (3.02 ± 0.85) and VSL#3 (3.84 ± 0.37) at 6 months. [Table 5(A,B)]
Discussion
In the present study rifaximin performed well overall in improving IBSSS and SGA for relief. However, the effect of rifaximin was no better than relaxation therapy in decreasing generalized ill-feeling at six months of therapy. Relaxation therapy has shown significant improvement at 6 months in all parameters when compared to VSL#3. The subjective global assessment took time to improve with all therapies till the sixth month. Treating IBS is important because the symptoms cause substantial impairment in Health-Related QOL, leading to increased use of health resources and reduced work productivity.15 There is a need for a non-pharmacological intervention that is easy to perform instead of a pill burden for this chronic ailment. Our study validated one such non-pharmacological intervention, relaxation therapy, which can be done without supervision once taught against the two established short term therapies, namely rifaximin and VSL#3. It would have been much better to have a placebo arm for such a study. However, for ethical reasons, it was not done. Epidemiologically IBS is 2-3 times more common in women than men. However, in our study, males represented 55% of the study population. A similar pattern of male predominance was seen in a community-based study from North India2. This could represent either a different demographic profile or the local cultural pattern. The ef?cacy of rifaximin in the treatment of IBS was evaluated in a randomized, double-blind, placebo-controlled, parallel-group study of 87 patients. In this study, patients received rifaximin 400 mg or an identical placebo thrice daily for ten days. Statistically signi?cant improvement in IBS symptoms was observed with rifaximin over place boduring the 10-week follow-up period among 80 of the 87 patients (36% vs. 21%, P = 0.02). This preliminary study was one of the ?rst to report the sustained bene?ts of IBS pharmacotherapy after cessation of treatment, a characteristic of rifaximin that separates it from other pharmacotherapies, with which symptoms return after treatment discontinuation.16 However, the follow up was only for ten weeks. In the Rifaximin in Abdominal Bloating and Flatulence Trial,17 which involved 104 patients with functional GI symptoms (74 ful?lled criteria for IBS), the percentage of patients with global symptom relief was higher with rifaximin than with placebo at the end of a 10-day course of therapy (41% vs.23%, p = 0.03). This difference persisted through the 30-day post-treatment observation period, with 29% of rifaximin-treated patients and 12% of placebo-treated patients reporting global symptom relief after this period (p = 0.02). In our study, the follow up of patients was for six months; there was an improvement in the IBSSS until the follow-up period. Evidence about probiotics in the treatment of IBS is type II (grade B). It is because efficacy has been reported with a single probiotic,with multiple species and occasionally even combined with prebiotics.18 Clinical studies using mainly lactobacilli and bifidobacteria alone or incombination, have been published.19 IBS pain subscale scores decreased significantly with VSL#3 over the treatment period in a study by Sonia Michail et al.20 The mean baseline pain score was 3.5±1.2 and decreased by 1.6±1.3 points at the end of the treatment period. A significant decrease also occurredin bloating, diarrhea, satiety, global scores, and QOL. However, these reportshave not studied the long term outcome of VSL#3 treated patients.21,22 In the present study, VSL#3 improved all three parameters studied, albeit inferior to the rifaximin over six months. Psychological treatments such as hypnotherapy, mindfulness, relaxation therapy, cognitive behavioural therapy, and patient education, have all shown to be effective in alleviating IBS related symptoms. These interventions target a patient’s appraisal of gastrointestinal (GI) sensations and symptoms, reductions in symptom-related anxiety, changes in arousal, and health behavior.23 Despite the relative effectiveness of these non-pharmacologic interventions, their implementation has been hindered by factors such as added cost, unavailability of trained clinicians, and a general bias towards pharmacotherapy among patients and providers.24 Blanchard et al. gave relaxation therapy for four weeks, and patients were followed up for the next four weeks.25 There was a statistically significant improvement in the GIsymptoms. Recent Cochrane Analysis 26 states that in relaxation therapy, Standardized Mean Difference (SMD)in symptom score improvement at two months was 0.50 (95%CI 0.02 to 0.98) compared with the usual care. The SMD in the improvement of abdominal pain at three months was 0.02 (95%CI -0.56 to 0.61) compared with usual care.26 However, long term follow up studies with this therapy are lacking. We have followed up the patients for six months, and our results reveal improvement in the IBS parameters until six months, better than the other two treatment groups involving pharmacological interventions.
Conclusion: Patients with IBS-D do better with rifaximin and VSL#3 in the short term. Patients respond better to relaxation therapy at the end of 6 months. Relaxation therapy is being a non-pharmacological and cost-effective therapy, could be implemented on a long-term basis.
Limitations of the study: This was an open-labelled, single-centre, hospital-based study. There was no placebo arm.
Future directions: The combination of relaxation therapy with rifaximin/VSL#3 could be studied as it would simultaneously target multiple pathophysiologies of this disease. Moreover, relaxation therapy once learned can be continued without supervision for a long time without the additional pill and financial burden.
References - Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology 2006; 130: 1480-1491 [PMID: 16678561 DOI: 10.1053/ j.gastro.2005.11.061]
- Makharia GK, Verma AK, Amarchand R, Goswami A, Singh P, Agnihotri A, Suhail F et al. Prevalence of irritable bowel syndrome: a community based study from northern India. J Neurogastroenterol Motil.2011 Jan;17(1):82-7 PMID: 21369496
- Salari P, Abdollahi M. Systematic review of modulators of benzodiazepine receptors in irritable bowel syndrome: is there hope? World J Gastroenterology 2011; 17: 4251-4257 [PMID: 22090780 DOI: 10.3748/wjg.v17.i38.4251]
- Quigley, E. and Quera, R. (2006) Small intestinal bacterial overgrowth: roles of antibiotics, prebiotics, and probiotics. Gastroenterology 130(2 Suppl. 1): S78–S90.
- Pimentel, M., Lembo, A., Chey, W., Zakko, S., Ringel, Y., Yu, J. et al. TARGET Study Group (2011a) Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med 364: 22–32.
- Majewski, M., Reddymasu, S., Sostarich, S., Foran, P. and McCallum, R. (2007) Efficacy of Rifaximin, a nonabsorbed oral antibiotic, in the treatment of small intestinal bacterial overgrowth. Am J Med Sci 333: 266–270.
- Lembo A, Pimentel M, Rao SS et al. Repeat Treatment With Rifaximin Is Safe and Effective in Patients With Diarrhea-Predominant Irritable Bowel Syndrome. Gastroenterology. 2016 Dec;151(6):1113-1121.
- Madsen K, Cornish A, Soper P, McKaigney C, Jijon H, Yachimec C, Doyle J, Jewell L, De Simone C. Probiotic bacteria enhance murine and human intestinal epithelial barrier function. Gastroenterology 2001; 121: 580-591 [PMID: 11522742]
- Collins, S. M., and Bercik, P. (2009).The relationship between intestinal microbiota and the central nervous system in normal gastrointestinal function and disease. Gastroenterology 136, 2003–2014.
- Clarke, G., Quigley, E. M., Cryan, J. F., and Dinan, T. G. (2009). Irritable bowel syndrome: towards biomarker identi?cation. Trends Mol. Med. 15, 478–489.
- Svedlund J, Sjodin I, Olloson JO, et al. Controlled study of psychotherapy in irritable bowel syndrome. Lancet 1983; ii: 589-91.
- Ostgaard H, Hausken T, Gundersen D and El-Salhy M: Diet and effects of diet management on quality of life and symptoms in patients with irritable bowel syndrome.Mol Med Rep. 5:1382–1390. 2012.
- C. Y. Francis, J. Morris & P. J. Whorewell .The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment PharmacolTher 1997; 11: 395–402
- Meyrat P, Safroneeva E, Schoepfer AM. Rifaximin treatment for the irritable bowel syndrome with a positive lactulose hydrogen breath test improves symptoms for at least 3 months. Aliment PharmacolTher. 2012 Dec; 36(11-12):1084-93.PubMed PMID: 23066911.
- Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of functional gastrointestinal disorders: prevalence, socio- demography, and health impact. Dig Dis Sci 1993; 38:1569-80.
- Pimentel M, Park S, Kane SV. Rifaximin, a nonabsorbable, gut-selective antibiotic, improves the symptoms of irritable bowel syndrome: a randomized, double-blind, placebo-controlled study. Ann Intern Med 2006; 145: 557–63.
- Sharara AI, Aoun E, Abdul-Baki H, Mounzer R, Sidani S, Elhajj I. A randomized double-blind placebo-controlled trial of Rifaximin in patients with abdominal bloating and ?atulence. Am J Gastroenterol 2006; 101: 326–33.
- Roberts LM, McCahon D, Holder R, Wilson S, Hobbs FD. A randomised controlled trial of a probiotic ‘functional food’ in the management of irritable bowel syndrome. BMC Gastroenterol 2013; 13: 45 [PMID: 23496803]
- Ki Cha B, Mun Jung S, Hwan Choi C, Song ID, Woong Lee H, Joon Kim H, Hyuk J et al . The effect of a multispecies probiotic mixture on the symptoms and fecalmicrobiota in diarrhea-dominant irritable bowel syndrome: a randomized, double-blind, placebo- controlled trial. J ClinGastroenterol 2012; 46: 220-227 [PMID: 22157240]
- Sonia Michail and HarshavardhanKenche Gut microbiota is not modified by Randomized, Double-blind, Placebo-controlled Trial of VSL#3 in Diarrhea-predominant Irritable Bowel Syndrome Probiotics Antimicrob Proteins. 2011 March; 3(1): 1–7.
- Kim HJ1, Vazquez Roque MI, Camilleri M, Stephens D, Burton DD, Baxter K, et al randomized controlled trial of a probiotic combination VSL# 3 and placebo in irritable bowel syndrome with bloating. NeurogastroenterolMotil. 2005 Oct;17(5):687-96.
- Camilleri M. Probiotics and irritable bowel syndrome: rationale, putative mechanisms, and evidence of clinical efficacy 2006 Mar;40(3):264-9.
- Lackner, JM.; McCracken, LM. Functional Pain Syndromes: Presentation and Pathophysiology. IASP Press; Seattle, WA: 2009. Cognitive-Behavioural Treatment of Functional Pain Disorders; p. 491-509.
- Lackner JM, Jaccard J, Krasner SS, Katz LA, Gudleski GD, Holroyd K. Self-administered cognitive behaviour therapy for moderate to severe irritable bowel syndrome: clinical efficacy, tolerability, feasibility. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2008; 6(8):899–906. [PubMed: 18524691]
- Blanchard EB, Greene B, Scharff L, Schwarz-McMorris SPRelaxation training as a treatment for irritable bowel syndrome. Biofeedback 1993 Sep; 18(3):125-32. PMID: 821850
- Zijdenbos IL, de Wit NJ, van der Heijden GJ, Rubin G, Quartero AO Psychological treatments for the management of irritable bowel syndrome (Review) 2009 The Cochrane Collaboration.
|