48uep6bbphidcol2|ID
48uep6bbphidvals|1913
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Acute arterial mesenteric ischemia is an uncommon but life-threatening clinical entity (mortality rate 50-70%)1. For this disease, A. J. Cokkinis has famously said, “the diagnosis is impossible, the prognosis is hopeless and the treatment useless”2. Etiology of acute arterial mesenteric ischemia includes acute thrombosis of chronic mesenteric atherosclerotic disease and acute embolization of previously disease-free mesenteric arteries3-7. Acute occlusion of the superior mesenteric artery (SMA) was the most common cause of acute arterial mesenteric ischemia, with a reported incidence rate of 8.6/100000/year8.
Open surgical repair was first described by Shaw from Massachusetts General Hospital in 19589. This procedure offers a direct assessment of bowel viability, resection of compromised bowel, and also enables immediate revascularization. Moreover, it eliminates variables in physician expertise (i.e., advanced catheter skills, imaging-related issues) that are encountered in the endovascular approach. Hence, it has been used since its inception. The literature review revealed that there is a scarcity of data related to outcomes of surgical treatment of SMA in patients with acute arterial mesenteric ischemia in the Indian scenario. It would be difficult to carry out prospective studies to evaluate the outcomes of surgical intervention of this life-threatening condition due to its low incidence and emergency presentation. Therefore, we preferred to design this retrospective study to evaluate the surgical outcomes in patients with acute arterial mesenteric ischemia.
Methods
This retrospective, observational and single-center study included patients who had undergone surgical intervention for acute arterial mesenteric ischemia due to thromboembolic occlusion of SMA between October 2010 to March 2017 depending upon inclusion and exclusion criteria of the study. Inclusion criteria were 1) patients diagnosed with acute arterial mesenteric ischemia due to thromboembolic occlusion of SMA; 2) patients who underwent surgical intervention with or without thromboembolectomy of occlusive SMA. However, patients who were diagnosed with chronic mesenteric ischemia or patients with acute arterial mesenteric ischemia due to occlusion of the inferior mesenteric artery or the celiac artery were excluded from the study.
Data were extracted from an electronic database to identify patients who underwent surgical intervention for acute mesenteric ischemia as a result of thromboembolic occlusion of SMA during the study period. The medical records of the patients were reviewed retrospectively to extract details that included demographic information, clinical presentation, diagnostic information, laboratory investigations, surgical intervention detail, and short-term outcomes of the surgical intervention.
Whenever patients presented to the hospital with a high index of suspicious for acute mesenteric ischemia, complete investigation including arterial blood gas monitoring and D-dimer was performed. A provisional diagnosis of bowel ischemia was made if there lactate acidosis, low bicarbonate, and high D-dimer. The diagnosis of acute mesenteric ischemia was confirmed with computed tomography (CT) angiography. Exploratory laparotomy was performed without any delay. If there were evidence of infract bowel, resection of non-viable bowel was executed. However, resection was avoided if there was the presence of ischemia without gangrene, and thromboembolectomy was performed using a Fogarty catheter (Edwards Lifesciences, Germany) to restore blood supply to ischemic bowel and to preserve as much bowel length as possible. Relook (or second-look) laparotomy was performed to identify persisting focal bowel ischemia 24-hours after the first surgical intervention in selected cases who were expected to have considerably reversible bowel ischemia. The decision to perform relook laparotomy was made at the time of primary surgical intervention, irrespective of clinical condition, or physical examination of the patient. The patients in whom the relook procedure was planned, only the skin incision was closed (while keeping the cut end of bowel outside through midline incision and the patient was shifted to an intensive care unit with ventilator support.
Short-term follow-up data included major and minor in-hospital morbidity and in-hospital mortality. Major in-hospital morbidity was defined as peritonitis, sepsis or septic shock, multi-organ failure, re-exploration, acute renal failure, and prolonged ventilation. Minor in-hospital morbidities included ileus, surgical site infection, or any other complications that required further treatment or prolonged hospital stay. Long-term follow-up data included short bowel syndrome, readmission to hospital for reoccurrence of mesenteric ischemia, and death at 1-year follow-up. Long-term follow-up data were obtained from either outpatient clinic visit records, subsequent hospital admission records, or telephone interviews. The diagnosis of sepsis was made when there was the occurrence of systemic inflammatory response syndrome (two or more of these clinical criteria: (1) temperature greater than 38°C or less than 36°C, (2) heart rate greater than 90 beats/min, (3) respiratory rate greater than 20 breaths/min or PaCO2 <32 torrs, and (4) white blood cell count >12,000 or <4000 cells/mm3 or > 10% immature (band) forms) in response to infection. If the patient with sepsis experienced hypotension (blood pressure <90 mm Hg or reduction >40 mm Hg from baseline) refractory to fluid resuscitation and hypoperfusion abnormalities (including lactic acidosis, oliguria, or altered mental status), the diagnosis of septic shock was made. Multiple organ failure was defined as two or more organ systems failing sequentially or at the same time in a patient with sepsis. Acute renal failure was defined as a urine output of 0.3 ml/kg/hour for 24 h or anuria for 12 hours. Patients who underwent relook laparotomy were considered to have prolonged or unplanned ventilation if they required ventilator support for more than 72 hours (3 days) after surgical intervention. However, those patients who did not undergo relook laparotomy were considered to have prolonged or unplanned ventilation if they required ventilator support more than 48 hours after surgical intervention. Respiratory failure was defined as the requirement of ventilatory support after extubation during the hospital stay of the patient. Short bowel syndrome was defined as need of parenteral nutrition or antidiarrheic medication at discharge. A relook procedure was defined as a planned control of bowel viability after open surgical intervention.
Statistical Analysis
Continuous variables are expressed as mean±SD, and categorical variables are expressed as frequency (percentages). Statistical analysis was performed using Statistical Package for Social Science (SPSS) version 20.0 (SPSS Inc, Chicago, IL).
Results
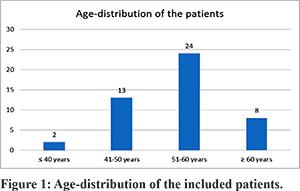
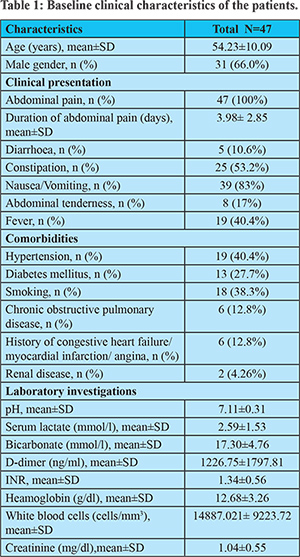
A total of 47 patients who were diagnosed and intervened surgically for acute arterial mesenteric ischemia due to thromboembolic occlusion SMA were included in this retrospective analysis. The age distribution of included patients is depicted in Figure-1. The majority of the patients were male (n=31; 66%). All the included patients experienced abdominal pain with an average duration of 3.98± 2.85 days. Abnormal lactate level (=2 mmol/l) and leukocytosis (>10,000 WBC/ccm) were noted in 25 and 28 patients, respectively. However, among 47 patients, 13 patients exhibited both the laboratory abnormalities, leukocytosis, and elevated lactate. Demographics and baseline clinical characteristics are shown in Table-1.
All the patients underwent exploratory laparotomy. The average time from clinical admission to operation was 8.34±8.210 hrs. Out of 47 patients, 33 patients were actively treated with open surgical revascularization with thromboembolectomy with/without bowel resection, whereas 14 patients underwent bowel resection without open surgical revascularization. Patients who underwent open surgical revascularization (n=33) were managed either with primary anastomosis (n=6) or with a stoma (n=27). None of the patients with primary anastomosis experienced an anastomotic leak. Refeeding was utilized in 23 patients with a proximal stoma (stoma at less than 50 cm from the duodenojejunal junction). Bowel reconnection was achieved in all patients with a stoma.
Except for three patients (who underwent open surgical revascularization), bowel resection was attempted in all the patients (n=44) during the first surgical intervention. Relook procedure was attempted in 17 (36.2%) patients. Among 17 patients who underwent relook procedure, 15 patients had been treated with open surgical revascularization. Gross improvement in bowel perfusion was observed (during second-look procedure) in 12 patients who had been treated with thromboembolectomy, and thereby bowel resection was not required during relook-procedure. Hence, a total of 5 patients required bowel resection during relook laparotomy (n=2 further bowel resection; n=3 resection at second-look only).
Table-2 summarised in-hospital and 1-year clinical outcomes. As a consequence of bowel resection, 14 patients experienced short bowel syndrome. Long-term parental nutrition was required in 9 (19.14%) patients. Prolonged or unplanned ventilation and sepsis were documented in 22 (46.8%) and 24 (51.5%) patients, respectively. Reexploration was performed in 2 (4.26%) patients. Other documented complications were diabetic ketoacidosis (n=3), septic encephalopathy (n=1), right renal artery emboli (n=1) and respiratory failure (n=1). In-hospital mortality was 8.5% (n=4) and cumulative one-year mortality was 36.2% (n=17). The cause of death during hospitalization included sepsis with multi-organ dysfunction (n=3) and postoperative severe myocardial infarction (n=1).
Discussion
This study summarises our experience of surgical intervention for acute mesenteric ischemia due to SMA occlusion. Acute arterial mesenteric ischemia due to thromboembolic occlusion of SMA has been associated with poor prognosis. Apart from high mortality, acute cessation of perfusion as a result of acute occlusion of mesenteric arteries leads to irreversible intestinal necrosis. The importance of early recognition of the condition and prompt aggressive surgical treatment has been iterated by several studies10-12.
Being a tertiary care center, our institute was most likely to receive referred patients. Hence, non-specific symptoms of acute mesenteric ischemia might have led to delayed diagnosis in the primary care center and consequently delayed referral to our tertiary care center (average duration of abdominal pain 3.98± 2.85 days). Delayed diagnosis has been reported in several studies. In Ottinger’s series of 103 patients (diagnosed with acute SMA occlusion), the duration of pain before diagnosis was found as high as 14 days13. Average time from presentation to surgical intervention was found to be 36±50 hrs in the study conducted by Char et al.10 In addition to delayed presentation, higher lactate concentration indicating transmural bowel infarction, was also present in our patients. Hence, open surgery was a prerequisite to perform in our study cohort to assess bowel viability and to resect non-salvageable bowel. Though we tried to preserve as much bowel length as possible, due to delayed presentation, overall, 44 (93.6%) of the patients required bowel resection during the first surgical intervention. Recent studies also reported that bowel resection needed to be performed in 31-93% of patients with acute mesenteric ischemia5,7,14-18. To avoid grave consequences of a non-salvageable bowel (peritonitis, sepsis, or multi-organ failure), the decision to perform relook procedure was made during the first procedure – independent of the clinical status of the patient or physical examination. Results showed that 29.4% of the patients required bowel resection during relook procedure, which reflected the utility of relook procedure without any significant consequences (due to relook surgery).
The rate of significant complications after bowel resection remains high. Gupta et al. reported 30-days postoperative (following bowel resection) morbidity and mortality rate as 56.6% and 27.9%, respectively19. Kougias et al. reported a 30-day mortality rate to be 31% following surgical revascularization in patients with acute mesenteric ischemia16. In our study, the in-hospital and cumulative 1-year mortality rate was 8.5% and 36.2%, respectively. Short bowel syndrome observed in 14 patients, particularly in those requiring resection more than 200 cm and proximal jejunum.
Recently, Plumereau et al. reported better survival in patients who underwent early revascularization (with or without bowel resection) as compared to those who underwent bowel resection only (mortality 10% vs. 68% at one-year follow-up)20. Park et al. also reviewed their experience of treating acute mesenteric ischemia and concluded that contemporary management (revascularization with open surgical techniques, bowel resection, and liberal use of relook procedure) resulted in improved survival in patients with thromboembolic occlusion7. The results of our study showed that 70.2% of patients (33/47) were actively treated with open surgical revascularization.
We acknowledge the limitations of the study. Limitations are majorly those factors that are inherent in any retrospective study. It is essential to identify true positive cases of acute mesenteric ischemia among clinically suspected cases. However, due to the retrospective nature of the study, it was impossible to retrieve this information. Additionally, we were unable to perform long-term radiological follow-up in all the patients.
Conclusion
The results of our study demonstrated that surgical intervention for acute arterial mesenteric ischemia due to thromboembolic occlusion of SMA is an effective treatment approach. Moreover, open surgical revascularization with thromboembolectomy can be considered in a selected cohort of patients without any added morbidity for the patients requiring exploration with extensive ischemia without peritonitis.
References
- Acosta S. Epidemiology of mesenteric vascular disease: clinical implications. Semin Vasc Surg. 2010;23(1):4-8.
- Cokkinis AJ. Intestinal ischaemia. Proceedings of the Royal Society of Medicine. 1961;54:354-6.
- Schoots I, Koffeman G, Legemate D, Levi M, Van Gulik T. Systematic review of survival after acute mesenteric ischaemia according to disease aetiology. British Journal of Surgery. 2004;91(1):17-27.
- Oldenburg WA, Lau LL, Rodenberg TJ, Edmonds HJ, Burger CD. Acute mesenteric ischemia: a clinical review. Archives of internal medicine. 2004;164(10):1054-62.
- Edwards MS, Cherr GS, Craven TE, Olsen AW, Plonk GW, Geary RL, et al. Acute occlusive mesenteric ischemia: surgical management and outcomes. Annals of vascular surgery. 2003;17(1):72-9.
- Endean ED, Barnes SL, Kwolek CJ, Minion DJ, Schwarcz TH, Mentzer Jr RM. Surgical management of thrombotic acute intestinal ischemia. Annals of surgery. 2001;233(6):801.
- Park WM, Gloviczki P, Cherry KJ, Hallett JW, Bower TC, Panneton JM, et al. Contemporary management of acute mesenteric ischemia: factors associated with survival. Journal of vascular surgery. 2002;35(3):445-52.
- Karkkainen JM, Acosta S. Acute mesenteric ischemia (part I) - Incidence, etiologies, and how to improve early diagnosis. Best practice & research Clinical gastroenterology. 2017;31(1):15-25.
- Shaw RS, Maynard EP, 3rd. Acute and chronic thrombosis of the mesenteric arteries associated with malabsorption; a report of two cases successfully treated by thromboendarterectomy. The New England journal of medicine. 1958;258(18):874-8.
- Char DJ, Cuadra SA, Hines GL, Purtill W. Surgical intervention for acute intestinal ischemia: experience in a community teaching hospital. Vascular and endovascular surgery. 2003;37(4):245-52.
- Kaleya RN, Sammartano RJ, Boley SJ. Aggressive approach to acute mesenteric ischemia. The Surgical clinics of North America. 1992;72(1):157-82.
- Boley SJ, Sprayregan S, Siegelman SS, Veith FJ. Initial results from an aggressive roentgenological and surgical approach to acute mesenteric ischemia. Surgery.82(6):848-55.
- Ottinger LW. The surgical management of acute occlusion of the superior mesenteric artery. Annals of Surgery. 1978;188(6):721-31.
- Ryer EJ, Kalra M, Oderich GS, Duncan AA, Gloviczki P, Cha S, et al. Revascularization for acute mesenteric ischemia. J Vasc Surg. 2012;55(6):1682-9.
- Alhan E, Usta A, Cekic A, Saglam K, Turkyilmaz S, Cinel A. A study on 107 patients with acute mesenteric ischemia over 30 years. International journal of surgery (London, England). 2012;10(9):510-3.
- Kougias P, Lau D, El Sayed HF, Zhou W, Huynh TT, Lin PH. Determinants of mortality and treatment outcome following surgical interventions for acute mesenteric ischemia. J Vasc Surg. 2007;46(3):467-74.
- Yun WS, Lee KK, Cho J, Kim HK, Huh S. Treatment outcome in patients with acute superior mesenteric artery embolism. Ann Vasc Surg. 2013;27(5):613-20.
- Beaulieu RJ, Arnaoutakis KD, Abularrage CJ, Efron DT, Schneider E, Black JH, 3rd. Comparison of open and endovascular treatment of acute mesenteric ischemia. J Vasc Surg. 2014;59(1):159-64.
- Gupta PK, Natarajan B, Gupta H, Fang X, Fitzgibbons RJ, Jr. Morbidity and mortality after bowel resection for acute mesenteric ischemia. Surgery. 2011;150(4):779-87.
- Plumereau F, Mucci S, Le Naoures P, Finel JB, Hamy A. Acute mesenteric ischemia of arterial origin: importance of early revascularization. Journal of visceral surgery. 2015;152(1):17-22.