48uep6bbphidcol2|ID
48uep6bbphidvals|1896
48uep6bbph|2000F98CTab_Articles|Fulltext
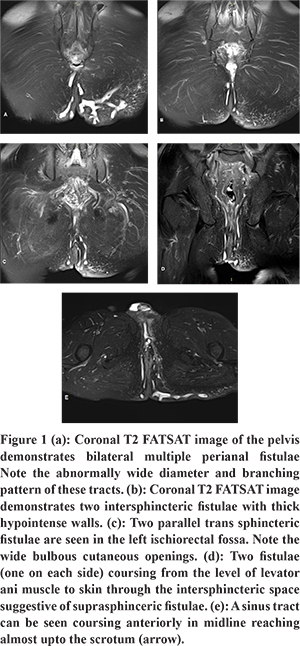
Tuberculosis remains a major health concern worldwide and is notorious for afflicting almost any organ and layer of the body especially in tropical countries. Ano-perianal tuberculosis is a rare gastrointestinal manifestation of TB with limited clinical, surgical and radiological literature. We describe a case of a 62 years old man with chronic history of multiple painful discharging wounds in perianal region. MRI evaluation revealed multiple patulous, complex fistulae of intersphincteric, trans-sphincteric and suprasphincteric morphology studded in the bilateral ischiorectal and ischioanal fossae and a sinus tract terminating in the anterior perineum. The number and morphology of these fistulae were markedly different from the routinely observed cryptoglandular fistulae and likewise histopathologic examination revealed tubercular pathology. Despite the tremendous use and efficacy of MRI in evaluation of perianal fistulae, there is virtually no literature concerning the MRI features of tubercular perianal fistulae.
Case Report
A 62 year old male presented to surgery department with complaints of multiple painful discharging wounds in the perianal region for the past three months. These resulted in painful defecation; however bowel habits and consistency were normal throughout the course of the disease. He had no abdominal, respiratory or neurologic complaints, however his son died of complications of pulmonary tuberculosis one year back. Associated complaints of generalized weakness, reduced appetite and sleep were present. No history of fever or any other documented comorbidities were present. On general examination the patient was thin, emaciated (weighing 51 kgs) with poor body hygiene. On examination of the perianal region multiple (atleast ten) erythematous discharging nodules and plaques were seen in perianal region and bilateral buttocks. Few of them were oozing foul smelling thick yellowish seropurulent discharge while others were covered with yellow projecting crusts. The skin adjoining the lesions was hyperpigmented and hyperkeratinised. No lesions were noted on the skin of scrotal sac or penis. Contrast enhanced MRI of the pelvis was requested to look for extent of the disease and communication with anorectum if any.
Multiplanar and multisequence contrast enhanced MRI of the pelvis was performed on 1.5T MR imaging system (TOSHIBA ExcelArt Vantage, Japan). Noncontrastfast spin echo T1 and T2 weighted sequences with and without fat suppression in axial, sagittal, coronal planes were acquired.Contrast (gadodiamide) enhanced MRI was done using T1 FATSAT sequence in axial and coronal planes.
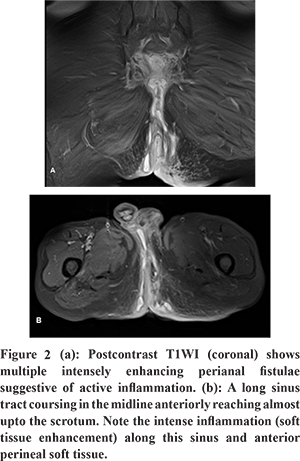
MRI revealed bilateral ischioanal and ischiorectal fossae to be studded with numerous fistulae. The fistulae were characteristically patulous with frequent ramifications, long courses and thick T2 hypointense walls (Figure 1a). The fistulae were of intersphincteric (Figure 1b), trans-sphincteric (Figure 1c) and suprasphincteric (Figure 1d) morphology. A sinus tract opening in the right ischioanal fossa was noted to course in the midline anteriorly reaching almost upto the scrotum (Figure 1e). Few fistulae were noted to cross the midline and/or join the fistulae of other side forming horse-shoe shaped fistulae (Figure 2c). Post contrast images demonstrated intense enhancement of the fistulae suggestive of active inflammation within them (Figure 2). No abscesses were noted in bilateral ischiorectal fossae or supralevator compartment. Biopsy fragments of the granulation tissue from the undermined edges of the external opening of the fistula demonstrated granulomas with langhans giant cells and caseation necrosis indicating tubercular pathology.
Discussion
Tuberculosis remains one of the major health concerns worldwide, especially in developing countries. Lungs are the most commonly inflicted organs. Among the varied extrapulmonary sites of infection, gastrointestinal tract tuberculosis accounts for less than 1% of all tuberculosis cases while anoperineal tuberculosis accounts for less than 1% of all the gastrointestinal tubercular infections.1 Though extremely rare, anoperineal tuberculosis is a debilitating form which imposes severe limitations on daily functioning of an individual. This coupled with the possibility of cure with anti-tuberculous drugs merits timely and accurate diagnosis of anoperineal tuberculosis.
PJ Gupta, has had immense clinical experience in evaluating ano-perineal tuberculosis in Indian subcontinent, and has described the various clinical presentations of ano-perianal tuberculosis asanal pain, fever and cough, anal or perianal ulcer with purulent exudates, a nonhealing wound around the anus, anal fistula (usually recurrent with multiple external openings, gross scarring and induration), perianal cutaneous ulcerations, acute perianal abscess, bleeding anal ulcer, anal stricture, hemorrhoidal thrombosis with fever and discharge, an associated anal lesion in HIV positive patient.2 Various typical and atypical morphological forms of ano-perianal tuberculosis include nonhealing anal orifice ulceration, anal ulceration with inguinal lymphadenopathy, pilonidal sinus, recurrent perianal growth, rectal stricture, anal fistula with tuberculous epididymitis, anal fistula with tuberculous salpingits, anal fissure, anal stricture, atypically located scrofuloderma, rectal submucosal tumor.2 Kraemer et al retrospectively analysed twenty cases of pathologically proven tubercular anal sepsis in an attempt to identify a set of specific clinical features. They concluded that tubercular anal sepsis (fistulas and abscesses) should be suspected in known pulmonary or extrapulmonary tuberculosis or if anal sepsis is persistent, recurrent or complex in nature.3 Thus a tubercular fistula-in-ano is usually complex (the track crosses >30% to 50% of the external sphincter, anterior in females, multiple tracks), recurrent and has a known or occult pulmonary or extrapulmonary tuberculous focus. Presently however, a tubercular fistula in ano is seldom diagnosed preoperatively. The prevalent method of diagnosis of tubercular fistula in ano still remains histologic and bacteriologic analysis of excised fistula or sample tissue.4 Early diagnosis of tubercular fistula in ano still remains a challenge.
MRI is increasingly used as a modality of choice for evaluating fistulous diseases of the anorectum. The advantages of MRI lie in the ability to define the course and extent of the primary and secondary tract, localize the internal opening, identify complications like abscesses, osteomyelitis, visceral communications and provide surgically relevant information. Majority of the existing MRI based studies and literature for evaluation of anorectal fistulae have focused only on cryptoglandular fistulae (nontubercular fistulae). Despite the increased accuracy and ever growing usage of MRI, there is virtually no radiological literature describing the MRI features of tubercular fistua in ano. Few recent case reports bearing MRI evidence describetubercular fistulae as complex in morphology and recurrent in nature which is in agreement to the clinical and surgical literature.5 Our case report reaffirms this and adds to the existing knowledge with much needed MRI based evidence.
Learning Point: Tubercular perianal fistulae and sinuses differ from typical cryptoglandular fistulae in that they are multiple, patulous with ramifications and long courses that can extend beyond the confines of ischiorectal and ischioanal fossae. MRI is an excellent modality to identify these features and provide a confident noninvasive diagnosis of tubercular perianal fistulae.
References
- Candela F, Serrano P, Arriero JM, Teruel A, Reyes D, Calpena R. Perianal disease of tuberculous origin: report of a case and review of the literature. Dis Colon Rectum. 1999;42:110e2.
- Gupta PJ. Ano-perianal tuberculosis. BratislLekListy. 2005;106(11):351-4.
- Kraemer M, Gill SS, Seow-Choen F. Tuberculous anal sepsis: report of clinical features in 20 cases. Dis Colon Rectum. 2000 Nov;43(11):1589-91.
- Yaghoobi R, Khazanee A, Bagherani N, Tajalli M. Gastrointestinal tuberculosis with anal and perianal involvement misdiagnosed as Crohn’ disease for 15 years. Acta DermVenereol. 2010;91:348–9.
- Oliveira Leonardo Guedes Leite de, PupoNeto João de Aguiar, Vieira Eduardo de Paula, Kim Monika Pereira, Flach Luciana da Costa, Almeida Barbara Cristina Rodrigues de. Proposed tuberculosis investigation and management protocol in complex and recurrent fistula-in-ano. J. Coloproctol. (Rio J.) 2015;35(2):113–119.