48uep6bbphidcol2|ID
48uep6bbphidvals|1881
48uep6bbph|2000F98CTab_Articles|Fulltext
Organ transplantation has been associated with a small but worrying risk of transmission of disease from donor to recipient. Initially reported for viral and bacterial infections following renal transplants1, similar reports are now mushrooming world over following liver transplantation.2 Whereas the common culprits, namely HIV, HBV, HCV, etc have been covered by screening protocols in the transplant evaluation, certain endemic infections are increasingly being reported to be transmitted via this route and maybe an unsuspected risk in specific geographical areas. Donor-derived infections pose an avoidable source of mortality and morbidity for the immune suppressed recipient. We present an interesting case of donor to recipient transmission of dengue virus following living donor liver transplant, with the donor developing hemorrhagic fever, and recipient having acute febrile illness. We also aim to elucidate the need for expansion of pre-transplant evaluation to accommodate screening for such endemic illness in future.
Case Report
The case involves a 64 year old male diagnosed with non-alcoholic steato-hepatitis (NASH) related cirrhosis with hepatocellular carcinoma (HCC), within Milan criteria prepped for transplant. He underwent right lobe living donor liver transplantation (LDLT), the donor being his healthy 28 year old son. All pre-operative factors for recipient and donor were optimized prior to transplant. Routine recipient work up included testing for HIV, HBV, HCV, CMV and VZV; all these tested negative. Pan cultures were also found negative. The donor on the other hand was tested for HIV, HBV, HCV and CMV; all of which were deemed negative. Neither donor nor recipient had any episode of fever within two weeks of scheduled transplant date. The donor was detected to have the rare Bombay blood group type.
Intra-operatively, a right lobe with subtotal middle hepatic vein (MHV) graft was harvested from the donor. With favorable vascular and biliary anatomy, the donor operation was uneventful, with no transfusion requirements in the immediate peri-operative period. In the recipient procedure, cold and warm ischemia times were restricted to 61 and 52 minutes respectively, and total procedure was completed within nine hours and five minutes. An acceptable graft-recipient weight ratio (GRWR) of 0.86 was obtained. Intra-operative blood product requirement was six units of packed red cells (PRBC), each unit having tested negative for routine bacterial, viral and protozoan infections.
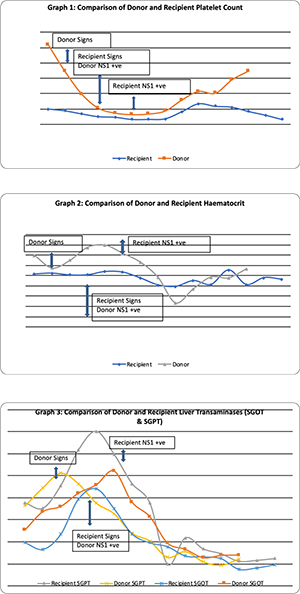
Post-operatively, the donor had a fever spike (103oF) on second post-operative day (POD), with associated drop in hemoglobin (Hb) and platelet (PLT) count. Blood and urine cultures done came back negative. Serum procalcitonin was elevated at 2.76. By POD 4, there was afebrile thrombocytopenia, PLT count (28,000). Dengue profile was sent, which showed NS1 antigen positivity. Hence under the supervision of Infectious disease expert, he was started on supportive therapy for dengue. Platelets persistently fell (14,000) despite therapy. On POD 9, he had sudden drop in Hb with hemorrhagic discharge from wound. PLT remained to be under 50,000 and he was thus transfused with packed red blood cells (PRBC) and single donor platelet (SDP) concentrates. He gradually responded to the above therapy and thereafter had an uneventful recovery period with no further drop in Hb or PLT counts. Donor was discharged healthy after a prolonged stay of 14 days.
The recipient, who was started on routine steroid and Tacrolimus immune-suppressive regime from POD 1, had similar incidents during his post-operative period. The PLT count witnessed a drop on POD 4 with associated rise in transaminases, without mounting a febrile response. Over the next two days, PLT count fell to as low as 13,000 with normal white cell counts. Intravenous Ganciclovir was started suspecting CMV infection. However, with no signs of clinical or hematological improvement, and simultaneously noting similar clinical occurrence in the donor as well, a Dengue profile was sent, which showed NS1 positivity for the recipient as well. The immune-suppression regime had mitigated the fever response, and thus made diagnosis difficult. He was also given supportive therapy, and required multiple PLT concentrate transfusions to overcome the acute stage. During the course of therapy, PLT counts returned to normal and liver functions stabilized by about POD 12. He overcame this episode, but later on in the course of hospital stay, he developed upper gastro-intestinal (GI) bleed requiring endotracheal intubation and ventilatory support. He then developed acute respiratory distress syndrome (ARDS), which soon progressed to multi-organ dysfunction syndrome (MODS), and he succumbed to illness on POD 30.
Discussion
Donor-derived disease transmission is reported to occur in less than 1% of transplants.3 Allograft donor-derived dengue viral transmission has been reported previously in living related renal transplants4, and is slowly creeping its way into living donor liver transplants as well, with two reports so far from North India2,5; a region known to be hyper-endemic to the disease, with increased frequency of outbreaks and ever changing circulating serotypes of the virus.
The transplant recipient, under the influence of immune-suppression, may not mount a febrile response. A close follow up of laboratory parameters would be required to ascertain the diagnosis. The atypical presentation in our case, of afebrile thrombocytopenia and elevated transaminases can be mistaken for acute cellular rejection or CMV infection. Accurate diagnosis of dengue required a concurrent detection of infection in the donor, thereby raising suspicion of disease transmission during organ transplant. Considering the average incubation period of dengue illness is between two to seven days, and that the donor is usually admitted one day prior to day of surgery, it is most likely that initial exposure to the virus happened in the community. Since it is nearly impossible to acquire any infection from the nearly sterile environment maintained within organ transplant intensive care units (ICU, donor to recipient transmission is the most plausible explanation.
References
- Davila PM, Fortun J, Velez RL, Norman F, de Oca MM, Zamarron P et al. Transmission of Tropical and Geographically restricted infections during Solid-Organ Transplantation. Clinical Microbiology Reviews. Jan 2008; 21(1): 60-96
- Saigal S, Choudhary NS, Saraf N, Kataria S, Mohanka R, Soin AS. Transmission of Dengue Virus From a Donor to a Recipient After Living Donor Liver Transplantation. Liver Transplantation 2013; 19:1413–1414.
- Ison MG, Nalesnik MA. An Update on Donor-Derived Disease Transmission in Organ Transplantation. American Journal of Transplantation 2011; 11: 1123–1130
- Tan FLS, Loh DLSK, Prabhakaran K. Dengue haemorrhagic fever after living donor renal transplantation. Nephrol Dial Transplant. 2005; 20: 447–448.
- Gupta RK, Gupta G, Chorasiya VK, Bag P, Shandil R, Bhatia V, Wadhawan M, Vij V, Kumar A. Dengue Virus Transmission from Living Donor to Recipient in Liver Transplantation: A Case Report. Journal of Clinical and Experimental Hepatology. 2016; 6:1: 59–61