Mary Dougherty1, Muhammad Bader Hammami2,3, Anuj Chhaparia2, Jinping Lai4, Christine Hachem1,21Department of Gastroenterology, 2Department of Internal Medicine, 3Division of Gastroenterology and Hepatology, 4Department of Pathology, Saint Louis University, Saint Louis University School of Medicine, St. Louis, MO, USA
Corresponding Author:
Dr Anuj Chhaparia Email: anuj.chhaparia@health.slu.edu, anujchhaparia@gmail.com
48uep6bbphidcol2|ID 48uep6bbphidvals|1880 48uep6bbph|2000F98CTab_Articles|Fulltext Intestinal adenomyomas, also known as myoepithelialhamartomas, are benign non-neoplastic tumor-like lesions characterized by glandular structures lined by cuboidal or tall columnar epithelium and surrounded by smooth muscle bundles. Reported cases of adenomyoma of the gastrointestinal tract have been largely confined to the stomach and duodenum, with lesions distal to the duodenum occurring less frequently. Here we report a case of adenomyoma of the jejunum that presented with anemia, along with a review of the literature.
Case Report
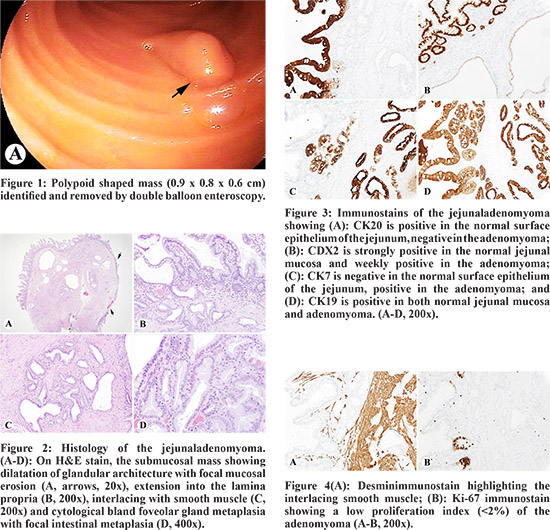
A 62 year old woman with history of heartburn and cholecystectomy presented for bronchial thermoplasty for treatment of asthma. She was incidentally found to have iron deficiency anemia. Anemia was evaluated with upper and lower endoscopy, and findings were negative for suspicious pathology or source of bleeding. Capsule video endoscopy revealed a pedunculated 10 mm polyp in the distal jejunum/proximal ileum. Endoscopic removal of the polyp was completed by double balloon enteroscopy. Grossly, the lesion was polypoid shaped measuring 0.9x0.8x0.6 cm (Figure 1). Microscopically, it was a well-circumscribed submucosal lesion composed of variably sized glandular structures surrounded by smooth muscle bundles. The glandular structures showed pyloric morphology and were lined by cuboidal or columnar epithelium with interspersed goblet cells and occasional Paneth cells (Figure 2). Immune-stains were performed with appropriate controls. The lesional epithelial component was strongly and diffusely positive for CK7 and CK19 and weakly positive for CDX2, but negative for CK20 (Figure 3). The smooth muscle component was positive for desmin and alpha-SMA. Ki-67/MIB-1, highlighting rare lymphocytes in the lesion and basal cells of the small intestinal mucosal epithelium (Figure 4). All pathologic features supported a final diagnosis of adenomyoma. The patient’s postoperative course was complicated by transient abdominal pain and bloating after the procedure. Abdominal X-ray was negative for free intra-abdominal air or perforation. Her pain resolved overnight and she was discharged the following morning. Upon follow-up one year later, she continues to do well, and the anemia has resolved.
 Discussion
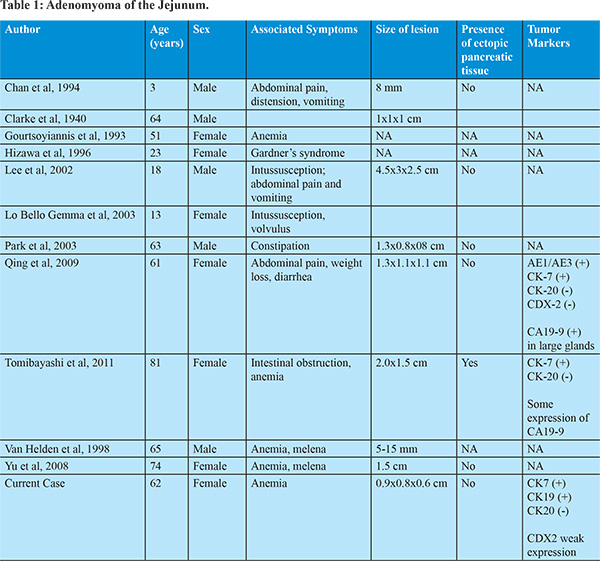
Myoepithelialhamartoma of the gastrointestinal tract was first described by Clarkein 1940.5 While the incidence of small intestine adenomyoma is relatively rare, the actual incidence is unclear because very few cases have been reported. Review of the literature reveals 34 reported cases in the small intestine,3,5-13,15-21,23-34 including the duodenum, ampulla of Vater, and ileum, with 11 well-documented cases reported in the jejunum (Table 1).3,5,9-10,16-17, 20-21,29,31,34 Of these cases, the patients were between the ages of three to eighty one years old, with six women and five men. While they are typically asymptomatic, symptoms of intestinal adenomyoma vary depending on the size, location of the lesion, and patient age. In the periampullary region, adenomyoma typically presents with biliary obstruction or abdominal pain, with reported cases of acute pancreatitis.14,22 Lesions in the ileum and jejunum have presented with intussusception and intestinal obstruction,29 but many reported cases have been incidentally detected. In the small intestine, intussusception is its most common complication, reported in 19 cases.1-3,6-8,11-13,15-20,24-25,27,32-33 Anemia has been reported in 11.7% of the cases described (4 cases). Most cases were surgically removed (26 cases), which may be attributed to a high number of laparotomies due to the adenomymoma presenting with intussusception, and a small percentage were removed endoscopically (3 cases). Microscopically, intestinaladenomyomas are submucosal tumors characterized by glandular structures lined by cuboidal or tall columnar epithelium and surrounded by bundles of smooth muscle.21 The differential diagnosis of this pathological presentation includes: enteritis cysticaprofunda, hamartomatous polyps in Peutz-Jeghers syndrome, adenocarcinoma, and pneumatosiscystoides. The pathogenesis of adenomyoma remains unclear, but the most widely accepted hypothesis is that it represents either a form of myoepithelialhamartoma or pancreatic heterotopia.26 The term ‘hamartoma’ refers to a focal but excessive overgrowth of cells indigenous to the particular site, while the term ‘heterotopia’ refers to microscopically normal cells that are present in an abnormal location. Clarke suggested that the classification of ‘adenomyoma’ be used only for lesions with exocrine-type ducts without ectopic pancreatic acini or islets surrounded by smooth muscle, and that the term ‘pancreatic heterotopia’ should refer to lesions with ectopic pancreatic acini or islets.5 In our case, we performed immunohistochemical testing in an attempt to increase our understanding of the origins of the adenomyoma. We detected the expression of CK7 and CK19, weak expression of CDX2, and the absence of CK20 expression. In general, CK7 is distributed in the pancreatic duct epithelium but is essentially absent in GI epithelium. CK20 is distributed in the GI epithelium but is absent in pancreatic duct epithelium.4 Thus, theimmunohistochemical features of the lesion are similar to that of the pancreatic duct epithelium and appear to support the heterotopic pancreas hypothesis. However, most reported cases of adenomyoma, including our present case, do not contain pancreatic tissue. In fact, the glandular structures showed pyloric morphology and were lined by cuboidal or columnar epithelium with interspersed goblet cells and occasional Paneth cells, suggesting a pyloric origin. Qing et al.(2009) and Tomibayashi et al. (2011) also reported cases of adenomyoma of the jejunum with goblet cells. Goblet cells were also found in a case of adenomyoma in a Meckel’s diverticulum.33
Conclusion
Adenomyoma of the small intestine is an extremely rare tumor largely unknown to most clinicians. While typically asymptomatic, symptoms of intestinal adenomyoma vary depending on size, location, and patient age. In our patient this lesion was likely the source of chronic GI bleeding manifesting as anemia. The prognosis of adenomyoma is excellent, with no evidence of recurrence or metastatic transformation in reported cases. Treatment of asymptomatic or bleeding adenomyomas is simple resection. Nevertheless, the pathogenesis of small bowel adenomyoma is not well understood due to its rarity, making further studies necessary.
References - Adetunji A, Healy D, et al. Adult intussusception caused by myoepithelialhamartoma in the small bowel: A case report. Int J Surg Case Rep. 2015; 8: 92–95.
- Bak YJ, Rolle U, Gfroerer S, Fiegel HC. Adenomyoma of the small intestine a rare pathological lead point for intussusception in an infant. Springerplus. 2014;18(3):616
- Chan YF, Roche D. Adenomyoma of the small intestine in children. Journal of Pediatric Surgery. 1994;29(12):1016-1018
- Chu PG, Weiss LM. Keratin expression in human tissues and neoplasms. Histopathology. 2002;40:403–439
- Clarke BE. Myoepithelialhamartoma of the gastrointestinal tract: a report of eight cases with comment concerning genesis and nomenclature. Archives of Pathology. 1940;30:143-152
- Gal R, Kolkow Z, Nobel M. Adenomyomatoushamartoma of the small intestine: a rare cause of intussusception in an adult. American Journal of Gastroenterology. 1986:81(12):1209-1211
- Gal R, Rath-Wolfson L, Ginzburg M, Kessler E. Adenomyomas of the small intestine. Histopathology. 1991;18(4):369-371
- Gonzalvez J, Marco A, Andujar M, Iniquez L. Myoepithelialhamartoma of the ileum: a rare cause of intestinal intussusception in children. European Journal of Pediatric Surgery. 1995;5(5):303-304
- Gourtsoyiannis NC, Bays D, et al. Benign tumors of the small intestine: preoperative evaluation with a barium infusion technique. European Journal of Radiology. 1993;16(2):115-125
- Hizawa K, Iida M, et al. Jejunalmyoepithelialhamartoma associated with Gardner’s syndrome: a case report. Endoscopy. 1996;28(2): 727
- Ikegami R, Watanabe Y, Tainaka T. Myoepithelialhamartoma causing small bowel intussusception: a case report and literature review. Pediatric Surgery International. 2006;22(4):387-389
- Khmou M, Znati K, et al. Synchronous adenomyomas of the ileum in an adult- an exceptional cause of intussusception. Clinical Case Report. 2015;3(7):578-581
- Kim CJ, Choe GY, Chi JG. Foregut choristoma of the ileum (adenomyoma) - a case report. Pediatric Pathology. 1990;10(5):799-805
- Kwon TH, Park DH, et al. Ampullaryadenomyoma presenting as a case of recurrent pancreatitis. World J Gastroenterology. 2007;13(2):2892-2894
- Lamki N, Woo CL, Watson AB, Kim HS. Adenomyomatoushamartoma causing ileoileal intussusception in a young child. Clinical Imaging. 1993;17(3):183-185
- Lee JS, Kim HS, Jung JJ, Kim JB. Adenomyoma of the small intestine in an adult: a rare case of intussusception. Journal of Gastroenterology. 2002;37(7):556-559
- Lo Bella Gemma G, Coradino R, Cavuoto F, Motto M. Myoepithelialjejunalhamartoma causing small bowel intussusception and volvulus. Radiol Med. 2003;105(3):246-249
- Mouravas V, Koutsoumis G, et al. Adenomyoma of the small intestine in children: a rare cause of intussusception: a case report. Turkish Journal of Pediatrics. 2003;45(4):345-347
- Nuño-Guzmán CM, Arróniz-Jáuregui J, et al. Adult intussusception secondary to an ileum hamartoma. World J. Gastrointest. Oncol. 2011;3(6):103.
- Park HS, Lee SO, et al. Adenomyoma of the small intestine: a report of two cases and review of the literature. 2003;53(2):111-114
- Qing X, Petrie BA, Bulson V, French S. Adenomyoma of the jejunum. Experimental and Molecular Pathology. 2009;86;127-130
- Rafiullah, Tanimu S. Adenomyomatous hyperplasia of the ampulla of Vater presenting as acute pancreatitis. BMJ Case Report. 2014.
- Rosenmann E, Maayan C, Lernau O. Leiomyomatoushamartosis with congenital jejunoileal atresia. Israel Journal of Medical Sciences. 1980;16(11):775-779
- Schwartz SI, Radwin HM. Myoepithelialhamartoma of the ileum causing intussusception. AMA Archives of Surgery. 1958;77(1):102-104
- Serour F, Gorenstein A, Lipnitzky V, Zaidel L. Adenomyoma of the small bowel: a rare cause of intussusception in childhood. 1994;18(2):247-249
- Takahashi Y, Fukusato T. Adenomyoma of the small intestine. World J Gastrointest Pathophysiology. 2011;2(6):88-92\
- Takeda M, Shoji T, et al. Adenomyoma of the ileum leading to intussusception. Case Rep Gastroenterol. 2011;5(3):602-609
- Tanaka N, Seya T, et al. Myoepithelialhamartoma of the small bowel: report of a case. Surg Today. 1996;26(12):1010-1013
- Tomibayashi A, Sasaki S, et al. Adenomyoma of the small intestine in an adult: report of a case. Surgery Today. 2011;41(8):1101-1105
- Ueyama N, Kuwashima S, et al. Ilealadenomyoma accompanied by primary peritonitis: report of a case. Surgery Today. 2001;31(9):826-829
- Van Helden SH, Jutten G, Van Hoey H, Dierick AM. Jejunalhamartoma as a rare cause of gastrointestinal haemorrhage. Histopathology. 1998;32(6):574-575
- Yamagami T, Tokiwa K, Iwai N. Myoepithelialhamartoma of the ileum causing intussusception in an infant. Pediatric Surg Int. 1997;12(2/3):206-207
- Yao JL, Zhou H, et al. Adenomyoma arising in a Meckel diverticulum: case report and review of the literature. Pediatric Dev. Pathol. 2000;3(5):497-500
- Yu HC, Lo GH, et al. Adenomyoma of the jejunum - a rare cause of gastrointestinal bleeding. J Chin Med Assoc. 2008;71(2)96-99.
|