Narendra Singh Choudhary, Neeraj Saraf, Rinkesh Kumar Bansal, Sanjiv Saigal, Nitin Sud, Aseem Kumar Tiwari, Arvinder S SoinMedanta Liver Institute, Medical Oncology and Blood Bank, Medanta, The Medicity, Gurgaon
Corresponding Author:
Dr Neeraj Saraf Email: neerajsaraf@hotmail.com
48uep6bbphidcol2|ID 48uep6bbphidvals|1877 48uep6bbph|2000F98CTab_Articles|Fulltext Thrombotic thrombocytopenic purpura (TTP) is a rare disease and diagnosis requires high index of suspicion. Timely diagnosis is very important as mortality is very high in untreated cases. We describe a case of living donor liver transplantation that had TTP, probably related to cytomegalovirus virus infection or tacrolimus.
Case Report
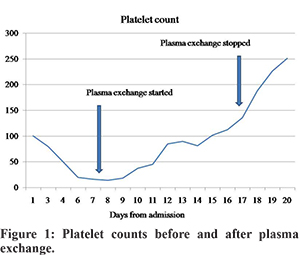
A 33 year old male underwent living donor liver transplantation (LDLT) for decompensated alcoholic cirrhosis, Child’s score 13/15, MELD score 32 before liver transplantation. He was diagnosed to have cytomegalovirus (CMV) viremia (1890 copies/ml) on day 21 after LDLT. He complained odynophagia, a gastroscopy was done which revealed esophageal ulcers, biopsy and immunohistochemistry was positive for CMV. He received injection ganciclovir initially followed by oral valganciclovir. Initially he was given tacrolimus, mycophenolate and steroids, it was modified in view of acute kidney injury to low dose tacrolimus (target trough level 4-6) and everolimus was added. He was admitted on post op day 100 with complaints of abdominal pain. His investigations revealed stable liver function tests; however, he had progressive thrombocytopenia (Figure 1) with anemia. A hematology opinion was taken. His work-up revealed normal iron profile, B12 and folate levels, raised lactate dehydrogenase (4232 U/L, normal up to 618), reticulocyte count 2.39%, peripheral smear showed 3.2% schistocytes and platelet count of 18000 cu/mm, serum ADAMTS13 activity was below normal. A diagnosis of thrombotic thrombocytopenic purpura (TTP) was made and tacrolimus was stopped. He was started on plasma exchange and his platelet count started to increase as shown in figure 1. He also had psychosis, which was improved with plasma exchange. He needed a total of 9 sessions of plasma exchange, mean plasma volume processed was 5.8 L (1.6 plasma volume), mean 13.7 fresh frozen plasma units used, average duration of plasma exchange was 183 minutes. At present his platelet count is 329000/cmm after 48 days of last session of plasmapheresies.
Discussion
Thrombotic microangiopathies are several diseases characterized by microangiopathic hemolytic anemia, thrombocytopenia, and variable organ involvement. Common thrombotic microangiopathies are TTP, Hemolytic-uremic syndrome and pregnancy related HELLP (pre-eclampsia/hemolysis, elevated liver enzyme levels, and low platelet) syndrome.1 TTP is very rare (< six cases per million per year) and timely diagnosis is important as mortality is 90% in untreated cases.2 Differential diagnosis include autoimmune hemolysis/Evans syndrome, disseminated intravascular coagulation, pregnancy-associated disorders (HELLP and eclampsia), hemolytic uremic syndrome, certain drugs and infections (generally viral including CMV).1 TTP is caused by de?ciency of von Willebrand factor (vWF) cleaving protein ADAMTS13. This deficiency may be congenital or acquired (by antibodies against ADAMTS13). Acute idiopathic TTP is the most common form of TTP.1 The ultra-large multimers of vWF released from endothelium are not cleaved in absence of ADAMTS13 and it causes spontaneous platelet aggregates at places of high shear (like microvasculature of the brain, heart and kidneys) which results in ischemia and thrombocytopenia due to consumption of platelets in platelet-rich thrombi. TTP should be treated as medical emergency as early death may occur after diagnosis.1 In a retrospective series of 18 thrombotic microangipathy (number of TTP not given), the authors found that overall rate of thrombotic microangiopathy after LDLT was 3.34 cases per 100 patient-years. Eight of these 18 patients (44%) died before improvement with plasmapheresis.3 Treatment consists of plasma exchange. CMV and tacrolimus have been shown to be associated of TTP.4,5 TTP should be suspected in presence of microangiopathic hemolytic anemia and thrombocytopenia in absence of other identifiable causes and a high index of suspicion is necessary for timely diagnosis and management.
References - Scully M, Hunt BJ, Benjamin S, Liesner R, Rose P, Peyvandi F, et al; British Committee for Standards in Haematology. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158:323-35
- Scully M, Yarranton H, Liesner R, Cavenagh J, Hunt B, et al. Regional UK TTP registry: correlation with laboratory ADAMTS 13 analysis and clinical features. British Journal of Haematology. 2008; 142: 819–826
- Nishi H, Hanafusa N, Kondo Y, Nangaku M, Sugawara Y, Makuuchi M, et al. Clinical outcome of thrombotic microangiopathy after living-donor liver transplantation treated with plasma exchange therapy. Clin J Am Soc Nephrol. 2006;1:811-9
- Maramattom bv, Patil R, Thomas P, Upendran B. Tacrolimus associated thrombotic thrombocytopenic purpura (TTP) and stroke in the young. Ann Indian Acad Neurol. 2015 ; 18: 126–127
- Neau D, Bonnet F, Viallard JF, Longy-Boursier M, Le Bras M. Thrombotic thrombocytopenic purpura and cytomegalovirus infection in an immunocompetent adult. Clin Infect Dis. 1997;25:1495-6.
|