48uep6bbphidcol2|ID
48uep6bbphidvals|1850
48uep6bbph|2000F98CTab_Articles|Fulltext
Zenker’s diverticulum (ZD) is a herniation of the posterior pharyngeal wall through a natural weakness between the inferior pharyngeal constrictor and the crico-pharyngeus muscle. It is the most common type of oesophageal diverticulum with a reported prevalence ranging between 0.01 to 0.11%. ZDs usually presents with dysphagia and regurgitation in middle-aged and elderly patients. Mediastinal extension of large ZD has rarely been described in literature.1,2,3 Esophageal intubation in patients with large ZDs is often very difficult. An endoscope may not be able to pass through the esophageal inlet in to the stomach because of esophageal compression and deviation. Visualisation of the esophageal inlet is sometimes not possible using traditional endoscopy in the left lateral position. In the supine position, we performed a successful endoscopic esophageal intubation in an elderly patient with a giant ZD. We also report one of the largest cases of ZD extending into the mediastinum up to the level of the aortic arch.
Case Report
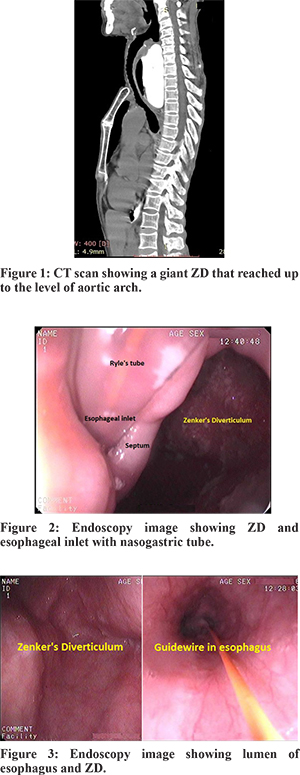
A 70-year-old female presented with dysphagia, weight loss and cachexia. Haemogram showed nutritional anaemia. Barium oesophagogram and CT-scan (Figure 1) demonstrated a massive ZD (Size 10.18 x 6.52 cm) extending into the mediastinum and reaching up to the level of the aortic arch. Contrast was barely visible in the oesophageal lumen. Attempts at endoscopy tried by other endoscopists were unsuccessful and therefore, the patient was referred to us. At our centre, endoscopy attempts in left lateral decubitus were unsuccessful due to preferential passage of the endoscope into the diverticulum. The patient was then turned to the supine position; slight angulation of the endoscope and a gentle pull back manoeuvre (nearly similar to ileocecal valve intubation) in the diverticulum was done to locate the oesophageal inlet (EI). We succeeded in visualisation of the EI and oesophageal intubation (Figure 2,3). We did not use sedation to reduce the risk of aspiration. A nasogastric tube was inserted (over a guide wire) into the stomach. However, the patient refused treatment and was lost to follow-up.
Discussion
ZD usually presents with dysphagia and regurgitation of retained food. It can also presents with weight loss, halitosis, and recurrent aspiration pneumonia. Large ZD can very rarely extend deep into the mediastinum.1,2,3 These cases can rarely presents with haemorrhage due to vascular erosion in the mediastinum.2 Cases of massive ZD extending into mediastinum and pressing against the aortic arch have rarely been reported.3
A large ZD forms in the midline (posterior to the oesophagus) and compresses the oesophagus. Therefore, visualisation of the EI and gastroscopy is sometimes not possible doing endoscopy in left lateral decubitus position.4 Compression of the oesophagus is reduced in the supine position and this facilitates the visualisation of the EI and esophageal intubation. There are a few methods that have been described for esophageal intubation in difficult cases of ZD.5,6,7 Under direct vision the catheter and guide wire can be advanced through the channel of the endoscope into the EI followed by insertion of the endoscope over the catheter/guide wire (where the EI is visualised).5,6,7 Swallow-assisted advancement of the catheter/wire blindly into the EI followed by insertion of the endoscope has been described in cases of non-visualisation of the EI5.
ZD is classified as small (< 2 cm), medium (>2 cm) and large (> 4-6 cm).1 Pouches of size larger than 10 cm are described as giant ZD.4 Treatment is recommended for symptomatic patients and requires myotomy of the cricopharyngeus muscle. Myotomy can be done by endoscopic or surgical methods. Endoscopic transoral cricopharyngeal myotomy performed with a laser or stapler is indicated for ZD of medium size. Surgical crico-pharyngeal myotomy with either diverticulectomy or diverticulopexy, via open or minimally invasive approach are usually reserved for larger ZDs.
References
- Balakrishnan V, Handwerker J, Verma SP. Giant Zenker diverticulum. Ear, Nose, Throat J. 2015; 94:310-11.
- Eaton J, Limsui D, Grover M. A man with dysphagia, aspiration, and hematemesis. Diagnosis: Hematemesis from a bleeding vessel in a large Zenker’s diverticulum. Gastroeneterology. 2011; 1407:e11–e12.
- Bock JM, Petronovich J, Blumin JH. Massive Zenker diverticulum. Ear Nose Throat J. 2012; 91: 319–20.
- Zhang X, Cheng S, Xu Y, Wang S. Treatment of giant pharyngoesophageal diverticulum by video-assisted thoracoscopy. Ann Thorac Surg 2014; 97:2184–6.
- Tsang TK, Buto SK. Catheter-guided endoscopic intubation: a new technique for intubating a difficult esophagus. Gastrointest Endosc. 1992; 38: 49–51
- Malik A, Chitnavis V, Epstein A. Use of a hydrophilic wire for esophageal intubation in Zenker’s diverticulum. Gastrointest Endosc. 1994; 40:523-4.
- Catalano MF, Raijrnan I. Wire guided endoscopic passage [Letter]. Gastrointest Endosc 1992; 38:728.