48uep6bbphidcol2|ID
48uep6bbphidvals|1809
48uep6bbph|2000F98CTab_Articles|Fulltext
Tuberculosis is known to afflict various organ systems and sites in human body. Abdomen is a common extra-pulmonary site for tuberculosis usually presenting aseither intestinal or peritoneal tuberculosis.1 However, involvement of gastroduodenal area is uncommon, which is believed to be because of high amount of gastric and pancreatic secretion present in these areas thatmay hinder the growth of mycobacteria. The literature studying duodenal tuberculosis is scanty and is usually in the form of case series or reports.2-5 We herein report a series of four patients with duodenal tuberculosis all of whom were diagnosed endoscopically and responded well to antitubercular therapy (ATT).
Case Series
Two of the four patients were males and the mean age of all patients was 35.25 years. The duration of symptoms prior to presentation varied from one and half months to 6 months. All patients had abdominal pain while three had features of gastric outlet obstruction (GOO). Other features were loss of appetite, loss of weight and fever (Table 1). All patients had a positive Mantoux test while one had evidence of healed old pulmonary tuberculosis on chest roentgenogram. Endoscopic findings included ulceration, nodularity, thickening of folds and narrowing of duodenal lumen (Figure 1A). Endoscopic diagnosis was possible in all patients but this required two attempts in two patients. In the second attempt, we used well biopsy technique (biopsy on site of previous biopsy) to take deeper tissue. In the other two patients the initial endoscopic biopsy itself yielded histological diagnosis.
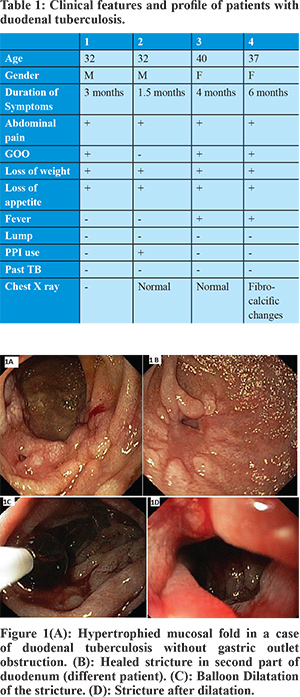
None of the patients had caseation while all had evidence of epithelioid granulomas (Table 2). None of the biopsies were positive for either acid fast bacilli or for TB-polymerase chain reaction. The quantitative C- reactive protein (CRP) levels were either normal or only mildly elevated in these patients (4.8-9.2). All patients were treated with standard four drugs (rifampin, isoniazid, pyrazinamide and ethambutol) for initial 2 months and two drugs for the later four months, i.e. Category I regimen. Only one patient needed endoscopic dilatation (Figure 1B, 1C, 1D) when the symptoms of gastric outlet obstruction did not improve after one month of ATT, and this procedure relieved the symptoms. None of the patients had reactive HIV serology.
Discussion
Gastroduodenal tuberculosis is an uncommon form of abdominal tuberculosis and is reported to mimic peptic ulcer disease and gastroduodenal malignancies.1 Traditionally the endoscopic diagnosis of this entity was believed to be unusual and surgery was both diagnostic and therapeutic.1,2 However, recent reports indicate that endoscopic diagnosis is feasible in a majority of cases. Indeed, authors have described use of endoscopic mucosal resection (EMR) which may increase the diagnostic yield.3,4 We haveinstead used well-biopsy technique for diagnosis in two patients in whom the initial biopsy was negative.5 This technique has been reported previously in diagnosis of ileocecal tuberculosis where the initial lesion is believed to be submucosal and surface mucosal biopsies may fail to yield the diagnostic histologic features.6 Since this method is easier to use than EMR, we suggest this should be the initial approach of choice to establish a diagnosis.
We also determined the CRP levels in these patients at the time of diagnosis which were elevated in three patients but the elevation was only mild. None of the patients had a positive AFB or PCR results suggesting a low bacterial load. We also used standard therapy with four initial drugs, as against the suggestion by some authors to add streptomycin atleast initially as absorption of oral drugs may be compromised.3,4
Unlike previous studies, only one of the three patients in this series with feature of GOO needed dilatation after one month of ATT. We delayed the dilatation to 1 month of ATT for two reasons, one in the hope that antitubercular therapy may itself relieve the obstruction and also the fact that with healing of ulcerations the dilatation may become safer. In a report of 10 patients of whom 9 underwent dilatation, there was a single occurrence of perforation.4 Although all patients in the present series had mucosal lesions, gastroduodenal tuberculosis can have submucosal or extrinsic lesions like lymph nodes which may cause luminal narrowing or bulge with normal overlying mucosa.1,7 The availability of endoscopic ultrasound provides a modality to access and sample such lesions.7 To conclude, endoscopic diagnosis is feasible in duodenal tuberculosis and patients respond well to the standard ATT while some patients may need dilatation of GOO.
References
- Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res. 2004;120:305-15.
- Rao YG, Pande GK, Sahni P, Chattopadhyay TK. Gastroduodenal tuberculosis management guidelines, based on a large experience and a review of the literature. Can J Surg. 2004;47:364-8.
- Puri AS, Sachdeva S, Mittal VV, Gupta N, Banka A, Sakhuja P, et al. Endoscopic diagnosis, management and outcome of gastroduodenal tuberculosis. Indian J Gastroenterol. 2012;31:125-9.
- Puri AS, Sachdeva S, Banka A, Sakhuja P. Tuberculosis of the duodenum: Clinical presentation, diagnosis and outcome. Indian J Tuberc. 2013;60: 83-88
- De A, Lamoria S, Dhawan S, Agarwal S, Sharma V. Duodenal tuberculosis: Dig deep to diagnose. Trop D. doi10.1177/0049475515613921
- Bhasin DK, Roy P, Sharma M, Singh K, Malik AK, Panigrahi D. Acid-fast bacilli in colonoscopic brushings. Lancet. 1991;338(8760):184-5. PubMed PMID: 1677082.
- Sharma V, Rana SS, Gunjan D, Chhabra P, Sharma R, Bhasin DK. Primary gastric tuberculosis mimicking a submucosal tumor. J Dig Endosc. 2015;6:130-2.