48uep6bbphidcol2|ID
48uep6bbphidvals|1806
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
In 1923, Dott was the first to describe the relationship between embryologic intestinal rotation and surgical treatment.1 In1936, William E. Ladd wrote the classic paper on treatment of malrotation. His surgical approach, now known as the Ladd procedure, remains the cornerstone of practice even today.2
Intestinal malrotation has traditionally been considered a disease of infancy.3-4 The actual prevalenceof malrotation in infants and children beyond the neonatal period is difficult to estimate, as such anomalies may remain asymptomatic and undetected throughout life. Intestinal malrotation is found in between 1 in 200 and 1 in 500 live births.3,5 But symptomatic malrotation occurs in only 1 in 6000 live births.6 High degree of suspicion should be kept while dealing with atypical GI symptoms in late childhood because it can lead to midgut volvulus and subsequently devastating intestinal necrosis.7
Normal embryonic rotation occurs in 3 stages, complete by 10-12 weeks of gestation, followed by fixation of mesentery, whichis onlycompleted soonbefore birth. Intestinal malrotation is a congenital anomaly occuring due to error of rotation of gut around superior mesenteric artery and anomalies in midgut fixation.The “omega” configuration predisposes to post-natal rotation about the narrow vascular mesenteric axis,leading to midgut volvulus with subsequent intestinal ischemia and necrosis. Due to maldevelopment, there can occur non-rotation and reverse rotation of gut. The commonest type encountered in children is narrow midgut mesenteric attachment to posterior abdominal wall that predisposes to volvulus and fibrous bands (of Ladd) coursing over 2nd and 3rd part of duodenum leading to duodenal obstruction.1-2
There is paucity of literature from Asian subcontinent on intestinal malrotation especially in children presenting later in childhood, which prompted us to study their clinical and radiological features as well as outcomes.
Methods
It is a retrospective study conducted in department of Pediatric Surgery between 2006 and 2015. Patients admitted with malrotation gut in childhood were included and analyzed for their clinical presentation, radiological diagnosis, operative procedures and surgical outcomes. However, patients of midgut malrotation associated with congenital diaphragmatic hernia, gastroschisis or omphalocele were excluded from the study.
Results
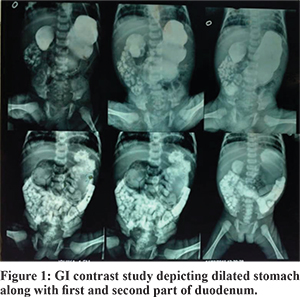
Total number of patients recruited in our studywas66.Of these,36 were neonates and 12 were between 1 and 5 year, 11 were between 5-10 year and 7 were between 10-14 year of age.Gender ratio (M:F) during infancy was 2.2:1 and beyond neonatal period was 2.8:1. All neonates presented with features of upper gastrointestinal tract obstruction like bilious vomiting and abdominal distention while presentation in later childhood was with atypical gastrointestinal symptoms like on and off bilious vomiting, pain in abdomen, malabsorption syndrome and failure to thrive. One of our patient presented with intussuception. In our series, 2 neonates(6%) presented with duodenal atresias and 4 neonates(12%) presented with jejunal atresias. Associated anomalies were observed in two patients,one had CHD and other had left PUJ obstruction. The diagnosis was confirmed with x-ray abdomen, USG abdomen and contrast study of upper GI tract (Figure 1). All patients were subjected to surgical correction of malrotation with Ladd’s procedure. The totalmortality was 4 in our series which counted for 6% of total patients.
All cases were operated, abdomen was opened through right transverse supraumblical muscle cutting incision and findings were identified. Volvulus was derotated,widening of mesenteric root done followed by division of ladd’s band and finally prophylacticappendicectomy was done and abdomen was closed in layers. We noticed significant mesenteric lymphandenopathy in some of the patients who presented late in childhood. But in 4 cases(two neonates, one infant and one child of 3 years of age) who presented with shock, there was midgut gangrene due to complete volvulus. Ladd’s procedure was done but gangrenous gut was not resected and was returned back to abdomen and abdomen closed. However, all 4 cases expired during post operative period due to sepsis. So in our study the incidence of midgut volvulus with gangrene was 6%. During post operative period,patients were allowed oral feeds after 72hrs once they started passing stool. Patients were discharged on 7th to 10th post operative day. Wound infection as seen in two patients was managed by daily dressing. On follow up, patients were reported to be doing well and gaining weight. Post operative adhesive obstruction was seen in two cases which was managed conservatively.
Discussion
Antenatal diagnosis is extremely difficult to make but a few case reports are available.8 None of the case was diagnosed antenatally in our series. Most of our patients presented in infancy (55%). However, as per literature, 50-80% of the patients present during infancyand malrotation gut can present at anyage.9-10 Nehra and Goldstein also emphasized on this fact. Similar findings were observed by Durkin et al.11
Malrotation may occur as an isolated anomaly or in association with other congenital anomalies; 30-62% of children with malrotation have an associated congenital anomaly. However, no genetic susceptibility or predisposing syndrome has been found to be associated with malrotation gut. Midgut volvulus when occur in utero cause variable degree of ischemic necrosis resulting into single and multiple atresias of small bowel.12 In our series, 2 neonates(6%) presented with duodenal atresias and 4 neonates(12%) presented with jejunal atresias. In a large series by Vecchia et al, 28% of infants with duodenal atresia and 19% of infants with jejunal atresia had malrotation.13 All children with diaphragmatic hernia, gastroschisis, and omphalocele were excluded from our study.
In our series, bilious emesis was the most prominent feature along with abdominal distension in neonatal age group leading to a prompt evaluation to achieve expedient diagnosis and treatment in line with findings of other case series.6 Malrotation in older children, however, can manifest with a broad range of symptoms ranging from an acute abdomen to vague and intermittent abdominal complaints and failure to thrive. Due to atypical GI symptoms, these patients are often misdiagnosed as suffering from milk allergy, malabsorption, celiac syndrome or even psychological disorders.
Sex ratio in the neonatal age group was 2.2:1 as expected but beyond infancy it was found to 3:1 in stark contrast to previous studies by Yanez et al where it hovers around 1:1.6,14
Diagnosis was mainly based on clinical presentation and radiological investigations. Initially children were subjected to X-ray abdomen leading to suggestive findings like paucity of gaseous shadows beyond 2nd part of duodenum or multiple air fluid levels. A gasless abdomen associated with abdominal distension or tenderness may be a sign of strangulated midgut volvulus.13 Doppler USG findings of a “whirlpool” or ‘swirl” sign of twisting of superior mesenteric artery is diagnostic of volvulus.16-17 All the patients except four who presented with complete volvulus were subjected to barium contrast studies. Barium mealfollow through showed gross dilatation of 2nd and 3rd part of duodenum with leakage of some dye beyond that part. Barium enema showed abnormal positioning of caecum. Definitive diagnosis was made on explorative laprotomy.
Unfortunately we lost four of our patients (6%) who presented with complete volvulus leading to gut gangrene and shock. Various recent case series shows mortality rates in adults and children operated on for intestinal malrotation ranging from 0-14%. Higher mortality rates are seen in cases with acute onset of midgut volvulus, delayed diagnosis, or the presence of intestinal necrosis.18-20 Children with other associated anomalies also have higher overall mortality rates. But the incidence of complete volvulus leading to gut gangrene is very less beyond infancy(3%). A report of 25 years experience demonstrated congenital cardiovascular disease in 27.1% of patients with intestinal malrotation; those patients had a morbidity rate of 61.1% after intestinal malrotation surgery.21
Conclusion
Midgut volvulus occurs more commonly in infants but its incidence becomes quite low beyond the period of infancy. Although rare, still the condition should be diagnosed early and treated in time to prevent morbidity and mortality.
References
- Dott N. Anomalies of intestinal rotation: their embryology and surgical aspects with report of five cases. Br J Surg. 1923;11:251-86.
- Ladd W. Surgical disease of the alimentary tract in infants. N Engl J Med. 1936;215:705-8.
- Ladd WE. Congenital Obstruction of the Duodenum in Children. N Engl J Med. 1932;206:277-80.
- Smith EI. Malrotation of the intestine. Welch KJ, Randolph JG, Ravitch MN, eds. Pediatric Surgery. 4th ed. St. Louis: MO: Mosby-Year Book; 1986. Vol 2: 882-95.
- Warner B. Malrotation. Oldham KT, Colombani PM, Foglia RP, eds. Surgery of Infants and Children: Scientific Principles and Practice. Philadelphia: Lippincott Williams & Wilkins; 1997. 1229.
- Nehra D, Goldstein AM. Intestinal malrotation: varied clinical presentation from infancy through adulthood.Surgery. 2011;149:386-93.
- Lampl B, Levin TL, Berdon WE, Cowles RA. Malrotation and midgut volvulus: a historical review and current contro-versies in diagnosis and management. PediatrRadiol.2009;39:359-66.
- Varetti C, Meucci D, Severi F, Di Maggio G, Bocchi C, Petraglia F et al. Intrauterine volvulus with malrotation: prenatal diagnosis. Minerva Pediatr. 2013;65:219-23.
- Millar AJ, Rode H, Cywes S. Malrotation and volvulus in infancy and childhood. SeminPediatr Surg.2003;12:229-36.
- Spitz L, Orr JD, Harries JT. Obstructive jaundice secondary to chronic midgut volvulus. Arch Dis Child. 1983;58:383-5.
- Durkin ET, Lund DP, Shaaban AF, Schurr MJ, Weber SM. Age-related differences in diagnosis and morbidity of intestinal malrotation. J Am Coll Surg.2008;206:658-63.
- Nixon HH, Tawes R. Etiology and treatment of small intestinal atresia:analysis of a series of 127 jejunal atresias and comparison with 62 duodenal atresias. Surgery.1971;69:41-6.
- Vecchia LKD, Grosfeld JL, West KW, Rescorla FJ, Scherer LR, Engum SA. Intestinal atresia and stenosis. Arch surg. 1998;133:490-7.
- Yanez R, Spitz L. Intestinal malrotation presenting outside the neonatal period. Archives of disease in childhood. 1986;61:682-5.
- Kassner EG, Kottmeier PK.Absence and retention of small bowel gas in infants with midgut volvulus:mechanism and significance.Pediatrradiol. 1975;4:28-30.
- Chao HC, Kong MS, Chen JY, Lin SJ, Lin JN. Sonographic features related to volvulus in neonatal intestinal malrotation. J Ultrasound Med. 2000;19:371-6.
- Pracros JP,Genin G,Tran-Minh VA,Morin de,Finfe CH,Foray Pet al. Ultrasound diagnosis of midgut volvulus: ?the whirlpool sign”.PediatrRadiol. 1992;22:18-20.
- Wallberg SV, Qvist N. Increased risk of complication in acute onset intestinal malrotation. Dan Med J. 2013; 60:A4744.
- Nagdeve NG, Qureshi AM, Bhingare PD, Shinde SK. Malrotation beyond infancy. J Pediatr Surg. 2012;47:2026-32.
- El-Gohary Y, Alagtal M, Gillick J. Long-term complications following operative intervention for intestinal malrotation: a 10-year review. PediatrSurg Int. 2010;26:203-6.
- Kouwenberg M, Severijnen RS, Kapusta L. Congenital cardiovascular defects in children with intestinal malrotation. PediatrSurg Int. 2008;24:257-63.