48uep6bbphidcol2|ID
48uep6bbphidvals|1793
48uep6bbph|2000F98CTab_Articles|Fulltext
Cutaneous metastasis from internal malignancy is rare. Furthermore, cutaneous metastasis from cholangiocarcinoma is extremely rare and none have been reported from India, to best of our knowledge.
Case Report
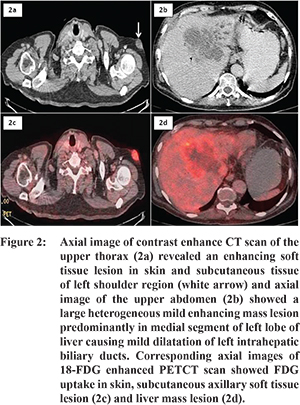
A 63 year old male, presented to us with history of weight loss, anorexia for last 2 months. Patient also had history of gradually progressive cholestatic jaundice since 10 days. On physical examination, patient was icteric, had multiple matted, firm, mildly tender, erythematous, subcutaneous nodule on the left axilla (Figure 1). Per abdomen palpation revealed hard, non-tender liver extending upto 5 cm below subcostal margin. Contrast enhanced CT scan (Figure 2b) revealed ill-defined heterogeneous mild enhancing mass seen predominantly involving medial segment of left lobe of liver causing narrowing and obstruction of left hepatic ducts with resultant mild dilatation of left intrahepatic biliary ducts s/o cholangiocarcinoma. CT scan image of upper thorax (Figure 2a) showed enhancing soft tissue lesion in skin and subcutaneous tissue of left axillary region suggestive of metastasis. Multiple enlarged portal, porto-caval, peripancreatic and mesenteric lymph nodes were present. Subsequent whole body PET CECT scan showed increased FDG uptake in left axillary region soft tissue lesion further confirmed the diagnosis of metastatic cholangiocarcinoma (Figure 2c,2d).

Laboratory analysis showed the following results: total bilirubin 24 mg/dL, with direct component 18.8 mg/dl, serum aspartate transaminase (AST)102 IU/L, alanine aminotransferase(ALT) 80 IU/L, alkaline phosphatase 523 IU/L, carbohydrate antigen 19-9 (CA 19-9) 1.2 ng/mL, carcinoembryonic antigen (CEA) 3.42 ng/mL, and alpha-fetoprotein (AFP) was 4.05 IU/mL.
Endoscopic ultrasound guided biopsy taken from portal lymph node revealed metastatic adenocarcinoma. Since skin metastasis is extremely rare in chalangiocarcinoma fine needle aspiration (FNAC) of skin lesion was taken which also revealed similar cytology (Figure 3).
Based on these findings; diagnosis of metastatic cholangiocarcinoma was made. The patient is being treated with systemic chemotherapy; to which he had partial response after three cycles of gemcitabine and oxaliplatin.
Discussion
Cutaneous metastases of cholangiocarcinoma are rare and have been reported to occur in only 0.4-5.3%, mainly at percutaneous biliary drainage site.
1,2 There are few case reports about distant cutaneous metastasis from cholangiocarcinoma.
3-5 Previous reports showed that the most common presentation of cutaneous metastases of cholangiocarcinoma is the nodular phenotype; other skin lesions described include ulcers, abscesses, and erythematous plaques.
3 Most nodular lesions are non-ulcerative, covered by a normal appearing epithelium, firm and painless; which results in some lesions being misdiagnosed as benign. Clinicians should therefore consider the possibility of cutaneous metastases in patients with history of malignancy when examining skin nodules.
The most common site of cutaneous metastasis in cholagiocarcinoma is abdomen (at percutaneous drainage site) than chest.
1,6 There are reports of scalp metastasis as well.
5 However to best of our knowledge subcutaneous axillary metastasis is being reported for the first time.
References
- Lee JH, Lee YJ, Chung JY, Jung MY, Park JH, Lee JH et al. A Case of Cutaneous Metastatic Cholangiocarcinoma on the Percutaneous Transhepatic Biliary Drainage Catheter Insertion Site. Ann Dermatol. 2015;27:220-1.
- Shorvon PJ, Leung JW, Corcoran M, Mason RR, Cotton PB. Cutaneous seeding of malignant tumours after insertion of percutaneous prosthesis for obstructive jaundice. Br J Surg. 1984;71:694-5.
- Lu C-I, Wong W-R, Hong H-S. Distant cutaneous metastases of cholangiocarcinoma: report of two cases of a previously unreported condition. J Am Acad Dermatol. 2004;51:S108-11.
- Hyun SY, Lee JH, Shin HS, et al, Lee SW, Park YN, Park JY. Cutaneous Metastasis from Cholangiocarcinoma as the First Clinical Sign: A Report of Two Cases. Gut Liver. 2011;5:100-4.
- Dogan G, Karincaoglu Y, Karincaoglu M, Aydin NE. Scalp ulcer as first sign of cholangiocarcinoma. Am J Clin Dermatol. 2006;7:387-9.
- Balzani A, Clerico R, Schwartz RA, Panetta S, Panetta C, Skroza N, et al. Cutaneous implantation metastasis of cholangiocarcinoma after percutaneous transhepatic biliary drainage. Acta Dermatovenerol Croat ADC. 2005;13:118-21.