48uep6bbphidcol2|ID
48uep6bbphidvals|1778
48uep6bbph|2000F98CTab_Articles|Fulltext
Incidence of primary small intestinal malignancies is exceedingly low and these are most commonly adenocarcinoma on histology and located in the second part of duodenum.
1 Primary squamous cell carcinoma (SCC) of the small intestine(SI) is an extremely rare condition with very few case reports in the literature. We report here a case of primary SCC of ileum treated surgically.
Case Report
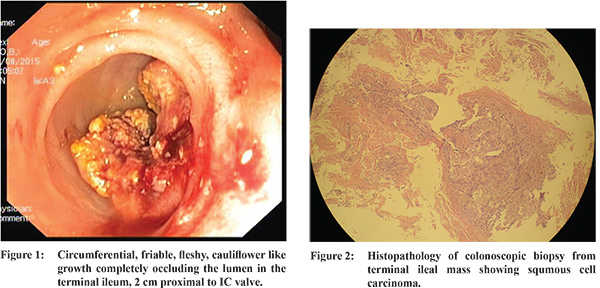
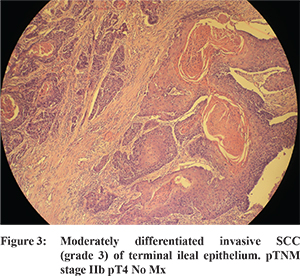
A 82 years old female with past history of laproscopic cholecystectomy eight years back and hysterectomy two years back for grade III uterine prolapse was admitted with periumbilical pain since 15 days, vomiting 3-4 hours after meals and constipation since 5 days. She had weight loss of 6 kgs in the last one-month. A plain X-ray film of abdomen was suggestive of small bowel obstruction following whicha contrast CT scan of abdomen and pelvis was performed which showed dilated jejunal loops with thickening of terminal ileal wall and collapsed ascending colon suggestive of obstruction in terminal ileum; no lymphadenopathy or ascites was found. Subsequently, colonoscopy was done which showed a circumferential, friable, fleshy, cauliflower like growth completely occluding the lumen in the terminal ileum, 2 cm proximal to IC valve (Figure 1). Routine laboratory assessment revealed iron deficiency anaemia while the tumour markers (CEA, CA 125) were not elevated. Histopathological examination of biopsy from the terminal ileal mass showed SCC (Figure 2). Patient was extensively evaluated to look for any primary site of malignancy (thorough clinical examination of head, neck and chest and a CT scan of thorax were normal). After accomplishing the preoperative readiness, patient underwent explorative laparotomy. Intraoperatively, a 3.8 x 6 cm mass was visualised in the terminal ileum for which quarter colectomy and resection anastomosis was done. Careful examination of vaginal vault was also done under anaesthesia to find for any primary lesion, which was normal. The patient was discharged on fourth postoperative day without any complications. The pathological examination of resected specimen revealed a mass of 5.5 cms in terminal ileum and incedentally found a Meckel’s diverticulum 5 cms long. Microscopic examination showed a moderately differentiated invasive squamous cell carcinoma (grade 3) arising from terminal ileal epithelium; regional lymph nodes and resection margins were free of tumour and meckel’s diverticulum was unremarkable. Pathological stage (pTNM) was IIb pT4 No Mx (Figure 3). Patient was not subjected to chemotherapy. She is doing well at three months of follow up with no evidence of recurrence.
Discussion
Metastatic SI malignancies are well known but primary SI malignancies are rare and amongst them primary SCC are extremely rare. Extensive search found 5 case reports of primary SCCs of small bowel (3 cases in duodenum (1-3), 1 in jejunum (4) and 1 in ileum (5). In a recent analysis of 1,312 consecutive pathologic specimens of SI only 3 cases (0.2%) of primary SCC were found.
6 It is difficult to differentiate between a primary SCC and a metastatic SCC based only on histopathology when it is found in the SI. Two differentiating points have been emphasized, first squamous metaplasia of the glandular epithelium favours it being the primary origin site and second, if there is little involvement of the mucosa, the lesion is more likely to be metastatic.
7 However a review of 100 metastatic carcinomas involving gastrointestinal (GI) mucosa found that metastatic carcinomas involving the mucosal surface of the intestines have a tendency to exhibit gross and histologic features mimicking primary tumours, especially when they originate from elsewhere in the GI tract.
8 They concluded that in situ growth cannot be taken as prima facie evidence of a primary neoplasm.Following mechanisms have been postulated for squamous differentiation: (1) malignant transformation of heterotopic rests of squamous epithelium in the submucosa; (2) aberrant differentiation of stem cells to squamous cells with subsequent malignant change; (3) squamous metaplasia of glandular cells with subsequent malignant change; (4) transformation of an adenocarcinoma into an epidermoid carcinoma.
9 We believe that our patient had a primary SCC of the terminal ileum without underlying adenoma, inflammatory disease, or duplication. As far as pathogenesis is concerned, we cannot exclude any of the four basic mechanisms proposed above. Clinical presentation of SCC of the ileum is similar to that of other ileal tumors. Optimal treatment and the prognosis are illusive because of the rarity of this condition. Surgery is the corner stone in the management ofthe disease.
10 Due to the small number of cases available in the literature the effects of chemotherapy and radiotherapy on the survival and recurrenceare unknown.
References
- Battal M, Bostanci O, Basak T et al. Pure squamous cell carcinoma of the duodenum. Case Rep Surg. 2015;2015:714640. doi: 10.1155/2015/714640. Epub 2015 Feb 16.
- Friedman E, Kwan MR and Cummins L. Squamous cell carcinoma of the transverse duodenum. Gastrointest Endosc. 1986;32:99-101.
- Von Delius S, Lersch C, Neu B et al. Squamous-cell carcinoma of the duodenum as a rare cause of upper gastrointestinal bleeding. Endoscopy. 2006;38:956.
- Sun DS, Shin OR, Ku YM et al.. Squamous cell carcinoma of the small bowel manifesting as a jejunal perforation: a case report. Int J Clin Exp Pathol. 2014;7(9):6345-9.
- Viamonte M and Viamonte M. Primary squamous-cell carcinoma of the small bowel. Report of a case. Dis Colon Rectum. 1992;35:806-809.
- Terada T. Malignant tumors of the small intestine: a histopathologic study of 41 cases among 1,312 consecutive specimens of small intestine. Int J Clin Exp Pathol. 2012;5(3):203-9.
- Mumtaz S, Ahmad Z, Fatima S et al..Squamous cell carcinoma in the small intestine. BMJ Case Rep. 2011;2011.
- Estrella JS, Wu TT, Rashid A et al.. Mucosal colonization by metastatic carcinoma in the gastrointestinal tract: a potential mimic of primary neoplasia. Am J Surg Pathol. 2011;35:563-572.
- Platt CC, Haboubi NY, Schofield PF. Primary squamous cell carcinoma of the terminal ileum. J Clin Pathol. 1991;44(3):253-4.
- A. Diffaa, Z. Samlani, Y. Narjis et al. The primitive squamouscell carcinoma of the third duodenum.Gastroenterology Insights. vol. 4, no. 1, 2012.