48uep6bbphidcol2|ID
48uep6bbphidvals|1746
48uep6bbph|2000F98CTab_Articles|Fulltext
Extramedullary hematopoiesis (EMH) is the proliferation of hematopoietic cells outside the bone marrow in response to decreased production or increased destruction of blood cells to satisfy the body’s demand. Insufficient production can be caused by bone marrow infiltrative disease (myelofibrosis or chronic myelogenous leukemia) and increased destruction by hemolytic anemias (thalassemia, hereditary spherocytosis or sickle cell anemia). Liver, spleen, posterior mediastinum, kidney and lymph nodes are the most common sites of EMH.
1,2 Although splenic involvement is relatively common in EMH, it usually presents in the form of diffuse infiltration and manifests clinically as splenomegaly. Focal involvement of spleen by EMH is extremely rare. We present a case of focal intrasplenic EMH in a middle-aged male which was initially misdiagnosed as a tubercular abscess.
Case Report
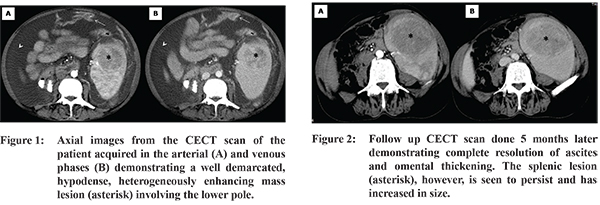
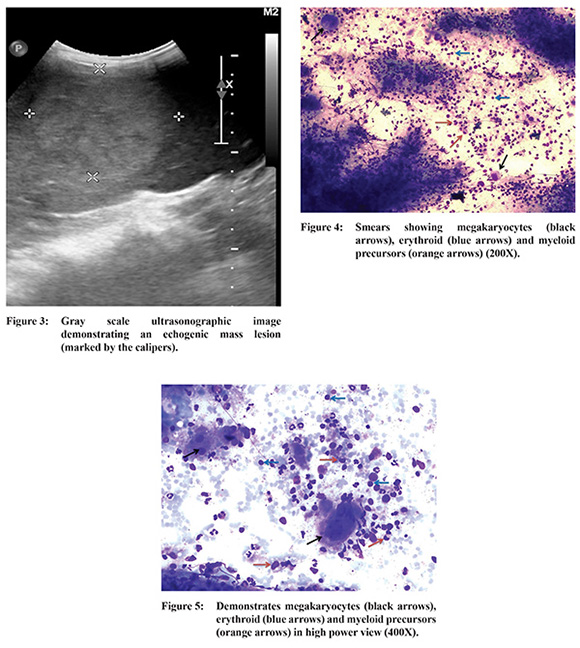
A 41-year old male presented to our out-patient department with complaints of pain in the left hypochondrium associated with low-grade fever, anorexia and gradually progressive abdominal distension for 1 month and loose stools for 8-10 days. General physical examination was unremarkable except for mild pallor. Systemic examination revealed a grossly distended abdomen with visible bulging of the flanks and a positive fluid thrill. Blood work was significant for leukocytosis (15.6x103 cells/µL; normal value (N) : 4 - 11x103 / µL) with a lymphocyte predominance (56%; N- 20-45%) and a low hemoglobin (9.5 g/dl; N: 13-17 g/dl). Ascitic fluid analysis showed a low serum-ascites albumin gradient with raised adenosine deaminase levels (48 U/L; N:<33 U/L) and leukocytosis (1630 cells/mm3 with 92% lymphocytes) raising the suspicion of abdominal tuberculosis. A contrast-enhanced computed tomographic (CECT) scan of the abdomen was carried out which demonstrated gross ascites with extensive omental thickening, abnormal peritoneal enhancement and multiple enlarged lymph nodes in the periportal, porto-caval, mesenteric and retroperitoneal region. In addition, there was evidence of splenomegaly with an approximately 5.5x4.9 cm sized, well-circumscribed, hypodense, heterogeneously enhancing mass lesion involving the lower pole of spleen (Figure 1). An omental biopsy was done which showed coalescing epithelioid cell granulomas with Langhan’s type of giant cells and focal necrosis. Ziehl-Neelsen staining showed presence of acid fast bacilli confirming the diagnosis of tuberculosis. In view of gross ascites, the splenic lesion was not biopsied for risk of bleeding and it was assumed to represent an evolving tubercular abscess. The patient was started on anti-tubercular therapy and kept on regular follow-up. He responded well to treatment with marked improvement in his symptoms within 3 months of commencement of therapy. Repeat imaging in the form of CECT was performed at 5 months which showed complete resolution of the ascites, associated omental thickening, peritoneal enhancement as well as lymphadenopathy. The splenic lesion, however, had increased in size and now measured 8.2 x 6.2 cm (Figure 2). Splenomegaly had also progressed markedly. Ultrasound correlation revealed a uniformly echogenic mass (Figure 3) with no overt vascularity on Doppler interrogation. Since the ascites had completely resolved, fine needle aspiration of the splenic lesion was done which revealed cellular smears composed of a mixed population of numerous megakaryocytic, granulocytic and erythroid precursor cells (Figure 4,5) consistent with EMH. The imaging studies were retrospectively reviewed for evidence of other foci of hematopoiesis, especially in paravertebral areas and bones, but none could be found. The patient was subsequently evaluated by a hematologist at another centre to rule out underlying hematological disorder where he underwent hemoglobin electrophoresis and was found to have homozygous delta-beta thalassemia.
Discussion
EMH is a compensatory response to ineffective erythropoiesis which is commonly seen in the haemoglobinopathies (especially thalassemia and sickle cell disease) and myelofibrosis. It favors certain sites such as the liver, spleen and the paravertebral regions of thorax. However, it can involve virtually any organ or tissue. Reported sites include abdominal viscera, kidneys, nasopharynx, paranasal air sinuses, intracranial structures and adrenal glands.
1,2 EMH is commonly recognized microscopically in the spleen and usually presents as splenomegaly. However, identification of focal lesions of EMH in the spleen on cross sectional imaging is extremely rare with only a handful of reported cases.
3,4 The splenic lesions can be solitary or multiple with the individual lesions being described as predominantly solid and well-defined. Pseudotumoral masses as large as 12 cm in size have been described.
3 Associated splenomegaly was found in almost all the cases.
Ultrasonography typically demonstrates an echogenic mass, whereas on CECT scan the lesion is hypodense and shows heterogeneous enhancement.
4 Appearances on magnetic resonance imaging can be variable depending on the amount of fat and the stage of evolution of hematopoietic tissue.
2 Active lesions appear isointense on T1-weighted images, hyperintense on T2-weighted images, and show some enhancement after administration of intravenous contrast medium. Chronic lesions may show low signal intensity on T1- and T2-weighted images without enhancement. On chemical shift imaging, these lesions usually appear hypointense on the in-phase images compared with that on opposed-phase images owing to the presence of iron.
5
References
- Christos S, Georgiades CS, Neyman EG, Francis IR, Sneider MB, Fishman EK et al. Typical and atypical presentation of extramedullary hematopoiesis. AJR. 2002; 179:1239-1243.
- Sohawon D, Lau KK, Lau T, Bowden DK. Extra-medullary haematopoiesis: a pictorial review of its typical and atypical locations. J Med Imaging Radiat Oncol. 2012;56(5):538-44.
- Matteuzzi B, Pieri L, Lisi F, Galimberti S, Campani D, Colagrande S. Imaging studies in extramedullary hematopoiesis of the spleen. Ann Hematol. 2014;93(2):347-9
- Singer A, Maldijian P, Simmous MZ. Extramedullary hematopoiesis presenting as a focal splenic mass: a case report. Abdom Imaging. 2004; 29(6):710-712.
- Elsayes KM, Narra VR, Mukundan G, Lewis JS Jr, Menias CO, Heiken JP. MR imaging of the spleen: spectrum of abnormalities. Radiographics. 2005;25(4):967-82.