48uep6bbphidvals|172
48uep6bbphidcol4|ID
48uep6bbph|2000F98CTab_Articles|Fulltext
Foreign substances, when introduced into the human body,may elicit inflammatory and foreign body giant cell reactions.Substances which may be introduced during surgery includetalc, suture, sponge, gauze, lint, glove powder, hemostaticmaterial, surgical clips, prosthetic implants, et cetera.Depending on the nature and the extent of the reaction elicitedby these foreign substances, they may cause lesionsaccompanied by varying symptoms. There have been reportsof surgically introduced foreign material causing lesions suchas intra-abdominal adhesions (secondary to suture and talcgranulomas),[1] tumour masses (textilomas orgossypibomas),[2] space-occupying lesions (especially in thebrain)[3] or even lesions mimicking metastasis in cancercases.[4] With this background in mind, we report a case withextensive post-operative foreign body giant cell reactionmimicking recurrence in an operated case of colon cancer.
Case history
A 45-year-old male patient diagnosed with carcinoma of thesigmoid colon, underwent left hemicolectomy with descendingcolon to rectum anastomosis and transverse loop colostomyin February 2008. Histopathology revealed features ofmoderately differentiated adenocarcinoma infiltrating into theserosa, with surgical margins free of tumour. One of the lymphnodes dissected from the specimen showed the presence ofmetastasis. The patient then received 5 cycles ofchemotherapy. Post-operative recovery was uneventful.
A routine follow-up CT scan, performed in August 2008revealed a circumferential mural thickening of the colonic wallin the region of the previously operated site. Colonoscopyshowed a nodular, partial lumen occluding growth, 20 cm fromthe anal verge. The lesion bled on touch and stronglysuggested recurrence of the carcinoma. Colonoscopic-guidedbiopsy from the lesion only revealed granulation tissue withno evidence of tumour; repeat biopsy was advised.
In view of the high degree of suspicion, exploratorylaparotomy with resection of the involved bowel segment wasperformed. Intraoperatively, thickening of the wall in the regionof the mid-descending colon was noted.
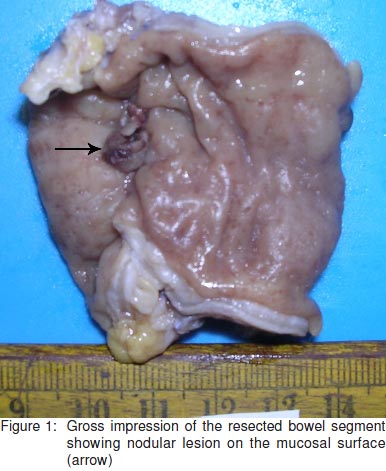
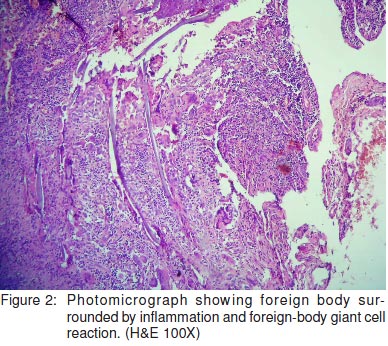
Grossly, the resected large bowel segment measuring 5cm in length showed nodular thickening on the serosal aspect.The corresponding mucosal surface showed two discretenodular lesions measuring 1.5 cm and 2 cm in diameter,respectively (Figure 1). The lesions displayed surfaceulceration and the cut surface was white and firm in consistency.The histological sections from the nodules revealed ulceration of the colonic mucosa with dense aggregates of inflammatorycells, consisting of lymphocytes, plasma cells and numerousforeign body type giant cells (Figure 2).
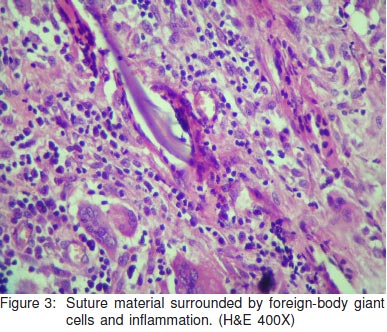
Amidst theinflammation, the suture material was identified within thecytoplasm of giant cells as well as lying extracellularly(Figure 3). In spite of extensive sampling of the resectedspecimen, no evidence of tumour was seen.The post-operativeclinical course of the patient was uneventful.
Discussion
Surgical procedures are an integral part of treatment in modern medical science.
They are, however fraught withinherent complications and side-effects. Surgeries invariablyexpose the human body to a large number of foreign material.These may be in the form of glove powder, gauze, lint, sutures,surgical clips, prosthetic implants or even locally appliedhemostatic material.
Absorbable sutures are used in surgical practice so asnot to elicit any significant foreign body reaction. However,suture granulomas are a well established histopathologicalentity. Shapiro[5] states that foreign body reaction to suturematerial shows a granulomatous response with histiocytesand foreign-body type giant cells around the suture material.Frequently, the suture material is seen within the macrophagesand the giant cells. Nylon suture, talc, and glove powder aredoubly refractile on polarising examination.[5] Luijendijk et al[1]undertook a study to determine the prevalence of foreign bodygranulomas in post-operative intra-abdominal adhesions andfound suture material to be the most common foreign materialassociated with post-operative intra-abdominal adhesions.They observed that suture granulomas were seen in 25% ofthe patients with past history of abdominal surgery.
Suturegranulomas can also produce lesions mimicking cancersclinically and even radiologically.[3] In the present case, suturematerial was identified within the cytoplasm of the foreign bodygiant cells as well as extracellularly. It was also discerned asbirefringrent on polarising examination.
Luijendijk et al[1] found starch granulomas in 5% of thepatients with post-operative intra-abdominal adhesions. Usingpolarised light, glove starch powder can be recognised by thetypical birefringrent Maltese crosses[1] in histological sections.Such Maltese crosses were not identifiable in the presentcase.
Gauze lint or cotton fibres, when retained in the body canelicit an exaggerated foreign body giant cell reaction. Thesemay mimic slowly growing soft tissue tumours (textilomas)and can attain enormous sizes. The radiological features ofsuch lesions have also been described.[6] Tinker et al[7] reported wo cases of granulomatous peritonitis in which a fibre-likeforeign material was identified on histology along withinflammatory and foreign-body giant cell reaction. These wereconfirmed as cellulose fibres from disposable surgical drapesand gowns that were birefringrent on polarisation and had atypical trilaminar configuration.
Resorbable and non-resorbable substances are used to achieve local hemostasis in the surgical bed intra-operatively.These may be composed of gelatin sponge, oxidised celluloseor microfibrillar collagen. Cotton- or rayon-based hemostatsmay also be used. These agents have been reported to causemass lesions, most commonly following intra-abdominalsurgery.[2] These may also produce symptomatic lesions likethe abscess, as reported by Ibrahim et al.[8] Histologicexamination shows a core of degenerating hemostatic agentsurrounded by inflammatory and foreign body reaction.[2] Nosuch material was used during surgery in the present case.
Blood, bile and material extruded from the gastrointestinaltract may also elicit a peritoneal inflammatory reaction causingpost-operative adhesions.[1] Such contamination is more likelyto occur in emergency laparotomies performed for acuteobstruction or perforation. In the present case, the surgerywas elective and adequately planned to avoid any such contamination.
Foreign chemicals can also be introduced into the bodyas a result of occupational and environmental exposure ordrug abuse. Such exposure however causes systemic effectswith functional impairment of the various organs.
To conclude, in spite of adequate precautions taken duringsurgery, inadvertent retention of foreign material inside thehuman body cannot be entirely avoided. Inflammatory andforeign body reactions to such materials can produce lesionsmimicking cancer, clinically and radiologically. It is thusimportant for the histopathologist to be aware of such entitiesand be acquainted with the histomorphology of identifiableforeign substances.
References
-
Luijendijk RW, de Lange DC, Wauters CC, Hop WC, Duron JJ,Pailler JL, et al. Foreign material in post-operative adhesions.
AnnSurg. 1996;223:242–8.
-
Ribalta T, McCutcheon IE, Neto AG, Gupta D, Kumar AJ, Biddle DA,et al. Textiloma (Gossypiboma) mimicking recurrent intracranialtumor.
Archives of Pathology and Laboratory Medicine,2004;128:749–58.
-
Epstein AJ, Russell EJ, Berlin L, Novetsky GJ, Lobo N, Miller SH, etal. Suture granuloma: an unusual cause of an enhancing ringlesion in the postoperative brain.
J Comput Assist Tomogr.1982;64:815–7.
-
Poyanli A, Bilge O, Kapran Y, Güven K. . Foreign body granulomamimicking liver metastasis.
Br J Radiol. 2005;78:752–4.
-
Philip E. Shapiro: Lever’s Histopathology of the Skin,
8th. Edition.Lipincott-Raven Publishers, Philadelphia 1997:pg.317.
-
Bellin M, Hornoy B, Richard F, Davy-Miallou C, Fadel Y, Zaim S, etal. Perirenal textiloma: MR and serial CT appearance.
Eur Radiol.1998;8:57–9.
-
Tinker MA, Burdman D, Deysine M, Teicher I, Platt N, Aufses AH Jr.Granulomatous peritonitis due to cellulose fibers from disposablesurgical fabrics.
Ann Surg. 1974;180:831–5.
-
Ibrahim MF, Aps C, Young CP. A foreign body reaction to SurgicelRmimicking an abscess following cardiac surgery.
Eur JCardiothorac Surg. 2002;22:489–90.